Prognostic Impact of Human Papilloma Virus Infection on Cervical Cancer Patients Reflected by p16ink4a Expression: Single Institution Experience
Download
Abstract
Background: Human Papilloma virus (HPV) is the main cause of cervical cancer. Infection with HPV can be reflected by overexpression of p16ink4a.
Aim of the study: we aimed at evaluating the expression of p16ink4a in cervical cancer patients and its prognostic significance.
Patients and methods: This retrospective registry and follow up study was conducted on 95 women diagnosed with cervical cancer. After screening of patients presented to our hospitals; 50 patients were eligible for inclusion in the study. P16ink4a was assessed by immunohistochemistry on archived tumor’s samples and correlation with different epidemiological, clinical and pathological data was performed. Prognostic impact of P16ink4a on overall survival (OS) and event free survival (EFS) was evaluated.
Results: Median age of patients was 55 years. The main presenting symptom was bleeding. Most of the patients presented with late FIGO staging 64% with stage IIIb and 10% with stage IIb. P16ink4a was positive in 80% of patients. Correlation between P16ink4a and different clinic-epidemiological data revealed positive significant correlation with tumor grade and tumor size (P values of 0.03 and 0.05 respectively). Considering the effect of p16ink4a expression and EFS and OS, our study failed to show any significant correlation.
Conclusion: The late stage at presentation of our population encourages the need for national screening program. The main cause of cervical cancer is HPV reflected by positive P16 similar to international literature. In our study the failure to reach a significant correlation with survival may be due the small sample size.
Introduction
Cervical cancer is the 4th common malignancy among women globally and the 14th in Egypt and the 11th among women [1].
A persistent infection with oncogenic Human papilloma virus (HPV) is recognized as the main cause of cervical cancer; with estimated around 80% of cases attributed to HPV serotype 16 and 18 and around 15% to other variants like 31, 33, 35, 45 and 52. Few cases were diagnosed with HPV negative. Usually HPV-negative cases are associated with adenocarcinoma histology, advanced stage at diagnosis and shorter survival [2].
The most common histology in cancer cervix is squamous cell carcinoma accounting for 85% of cases [3]. Histology plays an important prognostic role with adenocarcinoma and adeno-squamous histology has the worst survival and so should be treated more aggressively [4].
According to world health organization (WHO), comprehensive cervical cancer control includes primary prevention through vaccination against HPV, secondary prevention through screening programs and tertiary prevention through diagnosis and treatment of cancer cases [5].
Cervical cancer is the most preventable type of cancer. Effective prevention depends on HPV vaccination. In 2006, bivalent and quadrivalent vaccines were available with more than 90% prevention against the most common variants of HPV (16 and 18). In 2014, USA food and drug administration (FDA) approved the 9-valent vaccine to be administered for prevention of HPV and subsequently cancer cervix [6].
Human papilloma virus cannot be detected by culture methods, however HPV genome as well as transcripts can be achieved with hybridization procedures or DNA sequencing using polymerase chain reaction (PCR-based assay) [7].
There are various biomarkers for cervical cancer screening among them the p16ink4a demonstrated high sensitivity and specificity for squamous cell carcinoma [8]. High risk HPV subtypes have the ability to integrate into the replicating basal and para-basal epithelial stem cell genome resulting in overexpression of the p16ink4a protein [9].
A meta-analysis reported that the expression of p16ink4a is significantly associated with better prognosis in terms of longer disease free survival and overall survival [10]. In our study we aimed at evaluating the prevalence of HPV in cervical cancer patients using the p16NK4a expression and its prognostic significance.
Materials and Methods
This retrospective study included patients diagnosed with cervical cancer; presented to clinical oncology department and the cancer early detection unit in the maternity hospital, Ain Shams University, between the period of January 2014 and December 2018.
Patient with histological diagnosis of cervical cancer, with available paraffin blocks in the pathology archive and available medical records in the oncology department were included in the study.
During this period a total 141 patients were diagnosed with cervical cancer; of which 90 cases had complete medical records and pathological reports.
Only 50 paraffin blocks were available in the pathology archive with adequate tissue for the immuno-histochemical (IHC) study.
The patients’ details were extracted including the epidemiological data, clinical data, treatment details, pathological data as well as survival data.
Immuno-histochemical Procedures
Immuno-histochemical staining on paraffin blocks for all cases and controls was done for p16ink4a (Santa Cruz, sc-56330., Texas, USA) as per instructions given by manufacturers using automated immunohistochemical stainer. p16ink4a –immuno-stained slides were reported as negative or positive depending on the percentage of cells showing immune-positivity.
p16ink4a grading was done depending on the staining pattern and percentage of involved cells as follows: Positive (moderate or strong staining in more than 10% of epithelial cells) vs negative (less than 10% of epithelial cells with moderate or strong staining). Diffuse nuclear and cytoplasmic staining in 100% of tumor cells is designated as block positivity [11].
Statistical Analysis
The data was collected in excel sheet and programed and analyzed using Statistical software and the descriptive statistics, Chi-square test was used to assess differences in the distribution of categorical variables, Fisher’s exact test was used if the expected frequency was <5, Student T test, the Kaplan–Meier method was used for Overall Survival and progression-free survival (PFS) analyses. The log-rank statistical test is used to compere the differences in survival. The Cox regression method is used for Survival prognostic factor analyses. Hazard ratios were given with 95% confidence intervals (95% CI). All statistical analyses were performed using Statistical Product and Service Solutions (SPSS) software SPSS 22.0. A P value < 0.05 was considered statistically significant.
Results
Patients’ criteria (Table 1)
The mean age of the patients was 55; with 70% of patients were younger than 60 years. Two patients only (4%) were smokers and thirty patients (60%) were multigravida with 4 or more parity and 18 patients with 2 or 3 children.
| Min. | Max | Mean | SD | ||||
| Age (years) | 15 | 86 | 55.14 | 12.7 | |||
| N | % | ||||||
| Age (years) | < 60 | 35 | 70 | ||||
| >60 | 15 | 30 | |||||
| Smoking | Yes | 2 | 4 | ||||
| No | 41 | 82 | |||||
| Unknown | 7 | 14 | |||||
| Menopausal status | postmenopausal | 34 | 68 | ||||
| premenopausal | 16 | 32 | |||||
| Parity | nuligravida (NG) | 2 | 4 | ||||
| 2 | 8 | 16 | |||||
| 3 | 10 | 20 | |||||
| 4 or more | 30 | 60 | |||||
| Comorbidities | Yes | 25 | 50 | ||||
| No | 25 | 50 | |||||
| Previous gynecological surgery | Total Hysterectomy | 4 | 8 | ||||
| Subtotal hysterectomy | 3 | 6 | |||||
| No | 43 | 86 |
The main presenting symptom was bleeding in 80% of patients followed by pain and dyspareunia 16% of patients and no patient diagnosed with screening. The duration of symptoms ranged from 15 days to 4 years with median of 5 months.
Tumor characteristics (Table 2)
Patients presented with bulky disease 5 cm or more represented 52%. Most of the patients presented in advanced stages 10 patients stage IIb, 22 patients stage IIIb which represented 64% of the whole study population. Four patients presented with stump carcinoma after subtotal hysterectomy due to benign disease.
| Min | Max | Mean | SD | ||||
| Size (cm) | 3 | 9 | 5.65 | 1.51 | |||
| N | % | ||||||
| Size | < 5 cm | 24 | 48 | ||||
| > 5 cm | 26 | 52 | |||||
| FIGO staging | Ⅰ B | 6 | 13 | ||||
| *4 cases where not included in FIGO (stump carcinoma) n=46 | Ⅱ A | 4 | 8.7 | ||||
| Ⅱ B | 10 | 21.7 | |||||
| Ⅲ A | 1 | 2.2 | |||||
| Ⅲ B | 22 | 47.8 | |||||
| Ⅳ A | 2 | 4.3 | |||||
| Ⅳ B | 1 | 2.2 | |||||
| Pre-existing lesion | No | 39 | 78 | ||||
| HSIL | 8 | 16 | |||||
| Condyloma | 1 | 2 | |||||
| Polyp | 1 | 2 | |||||
| GIL | 1 | 2 | |||||
| Final histological type | Squamous cell carcinoma | 40 | 80 | ||||
| Adenocarcinoma | 5 | 10 | |||||
| Carcinosarcoma | 3 | 6 | |||||
| Small cell neuroendocrine carcinoma | 1 | 2 | |||||
| Adenosquamous carcinoma | 1 | 2 | |||||
| Grade | 1 | 2 | 4 | ||||
| 2 | 21 | 42 | |||||
| 3 | 20 | 40 | |||||
| Not reported | 7 | 14 |
Most of the patients (78%) had no pre-existing lesions in the cervix. Forty patients (80%) had squamous cell histology and 5 patients (10%) with adenocarcinoma. Other histology included small cell, carcinosarcoma and adenosquamous.
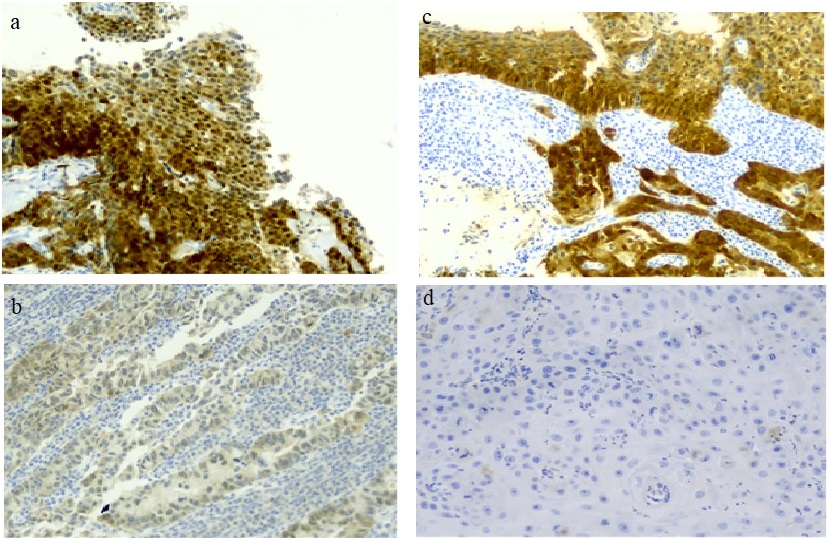
Eighty percent of the specimens were positive for P16; 22 patients with block diffuse positivity and 18 patients with focal nuclear positivity (Figure 1).
Figure 1. Different P16 Expression in our Population. a. A Case of Moderately Differentiated Squamous Cell Carcinoma with Strong Diffuse Positive Nuclear and Cytoplasmic p16INK4a Immunostaining (p16INK4ax200). b. A Case of Moderately Differentiated Adenocarcinoma Showing Diffuse Strong Cyoplasmic with Basal and Suprabasal Nuclear p16INK4 Aimmunostaining of the Covering Epithelium. The tumor cells in the underlying stroma shows diffuse strong cytoplasmic and nuclear p16INK4a immunostaining. (p16INK4ax200). c. A Case of Moderately Differentiated Cervical Adenocarcinoma with Mild Nuclear and Cytoplasmic p16INK4a Immunostaining in 30% of Tumor Cells (p16INK4ax200).d. A Case of Moderately Differentiated Squamous Cell Carcinoma with (negative p16INK4a expression). (p16INK4ax200).
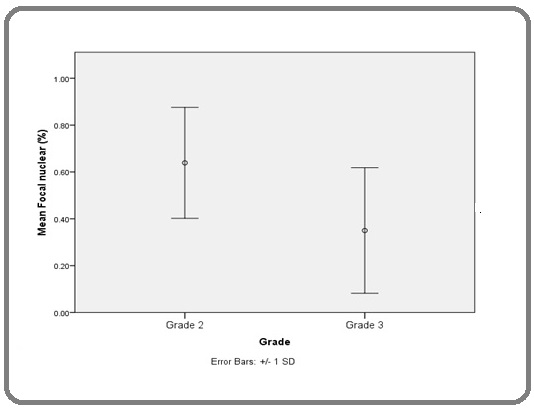
Correlation between P16 expression and different clinic-pathological parameters were done and revealed positive correlation between P16 focal nuclear percentage expression and the grade of the tumor (grade II tumor had mean percentage of expression of 64% compared to 35% in grade III tumors; (P 0.03) (Figure 2).
Figure 2.Mean Focal Nuclear Percentage Expression and the Grade of the Tumor (GII versus GIII, 0.64 ± 0.24 versus 0.35 ± 0.27, P 0.03).
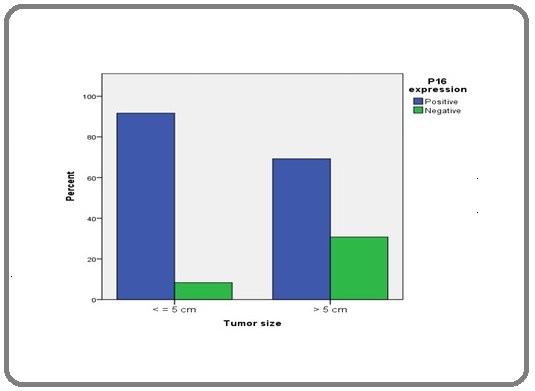
Also small tumors (5 cm or less) tended to be positive to P16 expression more than the larger tumors of more than 5 cm (p 0.05) (Figure 3).
Figure 3. Correlation between P16 Overall Expression and Tumor Size (p value = 0.05).
Treatment modalities
There were 42 (84%) patients received chemotherapy and 8 (16%) patients did not. The aim of chemotherapy was palliative in 7 patients and adjuvant in 35 patients.
There were 43 (86%) patients received radiotherapy and 7 (14%) patients did not. The aim of radiotherapy was definitive for 28 patients, adjuvant for 13 and palliative for 2 patients, moreover 19 patients received brachytherapy boost.
Survival analysis
After the study follow up period (median follow up period was 16 months), more than half of the study population (37 patients; 74%) had recurrence, progression or distant metastasis. 46 patients had survival data reported in the files and 4 patients lost follow up and were not included in the survival analysis.
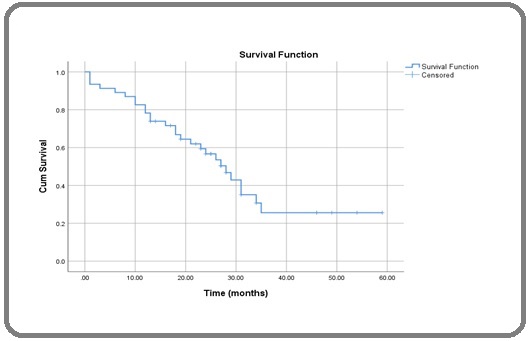
The median event free survival of the patients was 18 months and the median overall survival was 28 months as showed in Kaplan-Meir curves (Figures 4 and 5).
Figure 4. Event Free Survival (EFS) of the Whole Population (median 18 months).
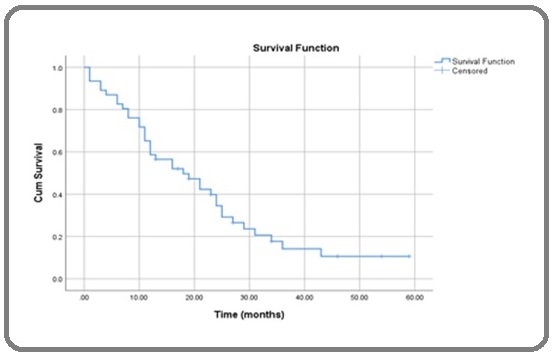
Figure 5. Overall Survival (OS) of the Whole Population (median 28 months).
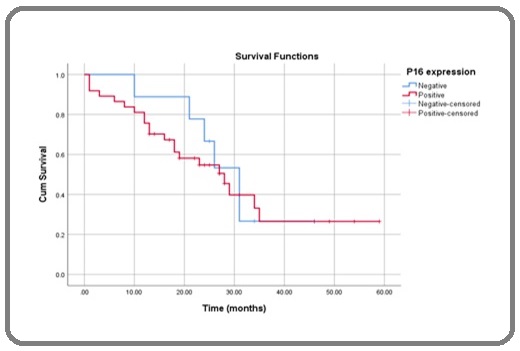
Correlation between P16 positivity and both EFS and OS revealed no statistical significance differences with P value of 0.351 and 0.209, respectively (Figures 6 and 7).
Figure 6. Correlation between P16 Expression and EFS (16 versus 24 months, p 0.35).
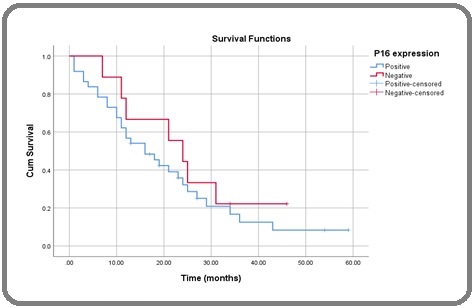
Figure 7. Correlation between P16 Expression and OS (28 versus 31 months, p 0.209).
Discussion
Persistent Human papillomavirus (HPV) infection is well-established as the major cause of most of invasive cervical cancers. It has been established that the E6 and E7 onco-proteins of high-risk HPVs, bind to the p53 and Retinoblastoma (Rb) tumor suppressor proteins, respectively, resulting in up-regulation of the tyrosine kinase P16ink4a. Overexpression of the p16 gene has been linked to high-risk HPV infection and high-grade CIN [12] The WHO recommends the use of HPV testing and p16 immunostaining for differentiation between HPV-associated and HPV-independent cervical cancer [13].
In this study, we reviewed 50 cases of invasive cervical cancer and evaluated p16 expression. We adjusted the survival analysis for age at diagnosis and FIGO staging (2018 version).This study was HPV genotype blinded, hence the significance of HPV genotypes on the clinical outcome of patients cannot be validated.
Mean age at time of diagnosis was 55 years, with 30% above age of 60, with slight difference in HPV associated cervical cancer which is more common at age of 49. Also 60% of the study population is multipara (≥4). This data go in hand with El-Moselhy et al [14] who stated that in Egypt, prevalence of the disease is very low for those below 35 years but significantly increase above that age. More than 15.0% of cervical cancer cases are found in women over 65. Also, significant association between high parity (>4) and cervical cancer was reported.
In the present study, IHC P16 expression in terms of diffuse block positive, focal nuclear positive or negative expression showed block positivity in 22 cases (44.0 %), focal nuclear in 18 cases (36.0%) and negativity in 10 cases (20.0 %); with overall 80% p16 positive and 20% p16 negative. Our results agreed with Sarwath et al [15] and Kaylani et al [16] trials, where anti-p16ink4a IHC correlation in SCC and other cervical tumors showed positive expression in 92% and 89% respectively.
Rokutan‐Kurata et al [17] concluded that the mechanism underlying the p16‐negativity in cervical squamous cell carcinoma is heterogeneous and may be contributed to the absence of a high‐risk HPV infection, the presence of a low‐risk HPV infection, CDKN2A gene methylation or deletion, and co‐infection of EBV.
There was no statistically significant association between age and P16 expression, where most block positive cases (36.0%) between 40-49 years, most focal nuclear cases (50%) between 50-59 years, and most negative cases (40%) between 60-69 years. This is data is similar to what Schwarz et al [18] reported that Patients with p16-negative tumors were older (mean age at diagnosis 65 vs. 52 years for p16-positive tumors; p = 0.01).
In our study the menopausal status, parity, clinical presentation, FIGO staging was not significantly correlated ith P16 expression. Where 68% of our population was postmenopausal and 60% with high parity (≥4). However the correlation between P16 expression and the histological subtype was approaching significance where 82.5% of the squamous histology was positive for P16 compared to 70% in the other histology subtypes. This agreed with Kaylani et al16 were no significant association between P16 expression and age at marriage (p = 0.951), age at menopause (p = 0.311), parity (p = 0.554), clinical symptoms/signs, stage of disease (p = 0.28).
Also agreed with Sarwath et al15, found that p16ink4a expression was directly proportional to the diagnosis of cervical tumors where 90.1% of SCC cases and 76.9% as Adenocarcinoma (AC) showed positive p16ink4a expression.
Amaro-Filho et al [19], disagreed with us, who analyzed the expression of Ki-67, p53 and p16ink4a in 130 diagnosed cases of cervical cancer, and its relative expression of these proteins together with clinical parameters with the stage of disease; found that p16 expression was independently associated with the tumor stage as High expression of p16 was more common in the advanced FIGO stages (p = 0.023).
In our study there was no significant correlation between P16 expression and event free survival (EFS) or overall survival (OS) and actually this data is controversial in literature where some studies reported same no significant data correlation with disease free survival or overall survival [18] and other trials were the expression of P16 was a good prognostic factor for overall survival (OS) [20] or disease free survival (DFS) [21].
Other data even reported the complete opposite results of P16 expression on the overall survival, like Putte and colleagues [22] where the P16 expression was negatively impacted the survival with P value of 0.036.
From the histopathological date in our study we found that presence of lymph node metastasis was independent negative prognostic factory for survival (p 0.037). this date is in concordance with Liu [23] and his colleagues’ data who suggested that Lymph node status has been reported as a prognostic factor for cervical cancer OS (P = 0.04) and PFS (P = 0.02). Also, Masoudi et al [24] reported that lymph node status (P < 0.0001), depth of stromal invasion (P = 0.0354) and tumor stage (P = 0.0355) were significant predictors of recurrence-free survival.
Finally our current study found that diffuse block positivity of P16 was significantly higher in the patients with positive LNs than those with negative LNs (71.4% vs 28.6%, P value = 0.02), Cox regression analysis shows that positive LN is significantly associated with higher risk of mortality (HR=2.611) (P value = 0.037).
We suggest that the cause of not reaching the significance in correlation between P16 expression and survival is due to the small sample size of our study and not testing the genotype of human papilloma virus (HPV) in our population.
In conclusion, Human papilloma virus which is reflected by the p16ink4a expression still the main leading cause of cervical cancer in our study population. The stage of presentation of cervical cancer in our study population is more advanced, which may reflect the need to implement screening programs and HPV vaccination campaigns. We failed to reach correlation between p16 expression and survival in our population which may be due to small sample size.
Limitations
The sample size was small and it is better to conduct another study in prospective manner. Also the HPV-DNA testing was not done on the paraffin blocks which is more accurate than the P16 to link the disease to HPV infection.
Recommendation
In spite of the different cultural, religious and economic situation of Egypt in comparison to the western countries, still HPV is the most common cause of cervical cancer in Egypt. Vaccination campaigns should be encouraged for both sexes of children starting at the age of 9 aiming at protection against HPV infection and subsequently the cervical carcinoma development.
Data availability
The unidentified datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
not applicable.
Funding
No fund was received for this study.
Ethical considerations
The study was approved by the ethical committee of Faculty of medicine, Ain Shams University IRB 00017585.
References
- ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World. Summary Report 17 June 2019 Bruni L, Albero G, Serrano B, et al . .
- HPV-Negative Cervical Cancer: A Narrative Review Arezzo F, Cormio G, Loizzi V, Cazzato G, Cataldo V, Lombardi C, Ingravallo G, Resta L, Cicinelli E. Diagnostics.2021;11(6). CrossRef
- Cervical cancer: A global health crisis Small W, Bacon MA , Bajaj A, Chuang LT , Fisher BJ , Harkenrider MM , Jhingran A, et al . Cancer.2017;123(13). CrossRef
- A comparison of pure adenocarcinoma and squamous cell carcinoma of the cervix after radical hysterectomy in stage IB-IIA Lee Y, Choi CH , Kim T, Lee Je, Kim B, Lee J, Bae D. Gynecologic Oncology.2011;120(3). CrossRef
- Adjuvant Human Papillomavirus Vaccine to Reduce Recurrent Cervical Dysplasia in Unvaccinated Women: A Systematic Review and Meta-analysis Lichter K, Krause D, Xu J, Tsai SHL , Hage C, Weston E, Eke A, Levinson K. Obstetrics and Gynecology.2020;135(5). CrossRef
- Cervical Cancer: An Overview of Pathophysiology and Management Johnson CA , James D, Marzan A, Armaos M. Seminars in Oncology Nursing.2019;35(2). CrossRef
- The natural history of human papillomavirus infection Sanjosé S, Brotons M, Pavón MA . Best Practice & Research. Clinical Obstetrics & Gynaecology.2018;47. CrossRef
- p16ink4a is a surrogate marker for high-risk and malignant cervical lesions in the presence of human papillomavirus Lakshmi S, Rema P, Somanathan T. Pathobiology: Journal of Immunopathology, Molecular and Cellular Biology.2009;76(3). CrossRef
- Procedure for immunocytochemical detection of P16INK4A antigen in thin-layer, liquid-based specimens Bibbo M, Klump WJ , DeCecco J, Kovatich AJ . Acta Cytologica.2002;46(1). CrossRef
- Prognostic significance of overexpressed p16INK4a in patients with cervical cancer: a meta-analysis Lin J, Albers AE , Qin J, Kaufmann AM . PloS One.2014;9(9). CrossRef
- p16 as a diagnostic marker of cervical neoplasia: a tissue microarray study of 796 archival specimens Lesnikova I, Lidang M, Hamilton-Dutoit S, Koch J. Diagnostic Pathology.2009;4. CrossRef
- Detection of human papillomavirus types in head and neck squamous cell carcinoma.Doctoral dissertation, University of the Free State Bulane A. 2019.
- Human papillomavirus-independent cervical cancer Fernandes A, Viveros-Carreño D, Hoegl J, Ávila M, Pareja R. International Journal of Gynecological Cancer: Official Journal of the International Gynecological Cancer Society.2022;32(1). CrossRef
- Cervical Cancer: Sociodemographic and Clinical Risk Factors among Adult Egyptian Females El-Moselhy EA , Borg HM , Atlam SA . Adv Oncol Res Treat.2016;1:106.
- Introduction of p16INK4a as a surrogate biomarker for HPV in women with invasive cervical cancer in Sudan Sarwath H, Bansal D, Husain NE , Mohamed M, Sultan AA , Bedri S. Infectious Agents and Cancer.2017;12. CrossRef
- Expression of P16 biomarker in squamous cell carcinoma of uterine cervix and its association with clinico-pathological parameters: A cross-sectional study Kalyani R, Kalyani R, Raghuveer CV , Sheela SR . Biomedical Research and Therapy.2020;7(9). CrossRef
- Uterine cervical squamous cell carcinoma without p16 (CDKN2A) expression: Heterogeneous causes of an unusual immunophenotype Rokutan-Kurata M, Minamiguchi S, Kataoka TR , Abiko K, Mandai M, Haga H. Pathology International.2020;70(7). CrossRef
- Prognostic significance of p16 expression in advanced cervical cancer treated with definitive radiotherapy Schwarz JK , Lewis JS , Pfeifer J, Huettner P, Grigsby P. International Journal of Radiation Oncology, Biology, Physics.2012;84(1). CrossRef
- A comparative analysis of clinical and molecular factors with the stage of cervical cancer in a Brazilian cohort Amaro-Filho SM , Golub JE , Nuovo GJ , Cunha CB , Levi JE , Villa LL , Andrade CV , et al . PloS One.2013;8(3). CrossRef
- P16 and HPV Genotype Significance in HPV-Associated Cervical Cancer-A Large Cohort of Two Tertiary Referral Centers Mata S, Ferreira J, Nicolás I, Esteves S, Esteves G, Lérias S, Silva F, et al . International Journal of Molecular Sciences.2021;22(5). CrossRef
- p16 expression in patients with cervical cancer and its prognostic significance: meta-analysis of published literature Huang K, Li LA , Meng YG , Fu XY . European Journal of Obstetrics, Gynecology, and Reproductive Biology.2014;183. CrossRef
- Expression of p27, p21, and p16 protein in early squamous cervical cancer and its relation to prognosis Putte G, Holm R, Lie AK , Tropé CG , Kristensen GB . Gynecologic Oncology.2003;89(1). CrossRef
- Outcome and prognostic factors in cervical cancer patients treated with surgery and concurrent chemoradiotherapy: a retrospective study Liu YM , Ni LQ , Wang SS , Lv QL , Chen WJ , Ying SP . World Journal of Surgical Oncology.2018;16(1). CrossRef
- Loss of p16 INK4 expression in invasive squamous cell carcinoma of the uterine cervix is an adverse prognostic marker Masoudi H, Van Niekerk DJ , Gilks CB , Cheang M, Bilek K, Fischer U, Ehlen T, Miller D, Horn LC. Histopathology.2006;49(5). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2023
Author Details