Accuracy of the Combination of TI-RADS and BETHESDA Regarding Histopathology of Thyroid Malignancy
Download
Abstract
Background and aim of the work: Thyroid carcinoma is a common type of cancer, making up 2.1% of all new cancers. Ultrasonography (USG) is used to check thyroid nodules. TI-RADS is a system that classifies thyroid nodules based on USG. High-risk nodules undergo fine-needle aspiration biopsy (FNAB), and the results are reported using the BETHESDA classification. This study aimed to determine how accurate TI-RADS and BETHESDA are together for diagnosing thyroid cancer.
Research design and methods: This observational study examined data from thyroid cancer patients. We assessed characteristic data comprising age, gender, TI-RADS, BETHESDA, and thyroid malignancy histopathology. An independent t-test and Fisher exact test assessed the relationships between TI-RADS, BETHESDA, and thyroid malignancy histopathology. Diagnostic tests were based on ROC curve analysis of FNAB (BETHESDA), USG (TI-RADS), and a combination of both in establishing a diagnosis of malignancy based on the results of histopathological examination.
Results: This study included 47 patients. FNAB (BETHESDA) was more accurate at 80.85% compared to USG (TI-RADS) and their combination. Similarly, FNAB (BETHESDA) had a higher sensitivity at 80.48% compared to USG (TI-RADS) and their combination. However, when FNAB (BETHESDA) and USG (TI-RADS) were combined, they had the highest specificity values, reaching 100.0%, compared to each examination alone.
Conclusions: The study found that while FNAB (BETHESDA) is accurate and sensitive, combining it with USG (TI-RADS) improves specificity, making it a valuable approach for clinical decision-making. This integration could lead to better diagnostic accuracy and patient outcomes by providing a more comprehensive assessment of thyroid nodules.
Introduction
Thyroid carcinoma is the most common endocrine malignancy, accounting for 2.1% of all new malignancies. The annual global incidence of thyroid cancer has steadily increased over the past few decades, nearly tripling from 4.9 per 100,000 in 1975 to 14.3 per 100,000 in 2009 [1]. The incidence of thyroid carcinoma is highest in countries with high human development index scores. This high number of cases is related to good surveillance and the use of high-resolution radiological methods for diagnosis. Ninety percent of thyroid carcinoma cases are dominated by differentiated thyroid carcinoma, which consists of papillary thyroid carcinoma and follicular thyroid carcinoma [2].
Ultrasonography (USG) is the primary investigation in evaluating thyroid nodules. The Thyroid Imaging Reporting and Data System (TI-RADS) is a risk stratification system based on USG to classify thyroid nodules. Patients with high-risk TI-RADS categories undergo fine-needle aspiration biopsy (FNAB), and the findings are reported according to the BETHESDA (The Bethesda System for Reporting Thyroid Cytopathology, TBSRTC) classification. The standard diagnostic terminology agreed upon by pathologists worldwide is the classification-based evaluation known as BETHESDA. An advantage of reporting a diagnosis using this system is that BETHESDA scoring can provide an overview of the risk of malignancy with recommendations for clinical management according to the category [3, 4]. The BETHESDA categories are used to determine the malignancy risk. Data regarding the sonographic classification of thyroid nodules and their cytological correlation with the final histopathological diagnosis are still scarce in Indonesia [5-7]. FNAB reduces the number of unnecessary thyroid surgeries for patients with benign nodules and accurately triages patients with thyroid cancer for appropriate treatment [8-10].
Based on this background, we studied the accuracy of the combination of TI-RADS and BETHESDA classifications concerning thyroid malignancy histopathology. We aimed to determine the accuracy of each examination so that it can be applied, especially in areas with limited facilities.
Materials and Methods
This research used an analytical observational method with a cross-sectional study design. It examined the relationship between independent variables (TI-RADS and BETHESDA) and the dependent variable (thyroid malignancy histopathology). The sampling technique employed was non-probability sampling using a total sampling method. The research sample consisted of secondary data extracted from the medical records of thyroid malignancy patients at Dr. Wahidin Sudirohusodo Central General Hospital in Makassar City from January 2019 to December 2023. The patients included in this study were those diagnosed with thyroid malignancy at Dr. Wahidin Sudirohusodo Hospital from 2019 to 2023, who had undergone both USG and FNAB examinations, followed by histopathological examination. Excluded were patients with thyroid malignancy who had not undergone USG and FNAB examinations, those with thyroid malignancy who had not undergone surgery, and individuals with tumors in other organs.
The factors assessed in this study were age, gender, TI-RADS, BETHESDA, and thyroid malignancy histopathology. A score was assigned for features noted in each ACR TI-RADS category: (1) normal thyroid gland, (2) benign lesions, (3) probably benign lesions, (4) suspicious lesions, and (5) probably malignant lesions. The BETHESDA classification is based on six cytologic categories: nondiagnostic, benign, atypia or follicular lesion of undetermined significance (AUS), suspicious for follicular neoplasm, suspicious for malignancy, and malignant. Thyroid malignancy histopathology encompasses malignancies arising from the thyroid parenchymal cells and is classified into four main types: papillary thyroid carcinoma, follicular thyroid carcinoma (FTC), medullary thyroid carcinoma, and anaplastic or undifferentiated thyroid carcinoma (ATC).
All research data were collected and tabulated in Microsoft Excel. The statistical analysis used SPSS version 27.0. The data obtained from medical records were collected and processed to obtain the distribution of the number and percentage of each variable under investigation using descriptive statistics. An independent t-test and Fisher exact test assessed the relationships between TI-RADS, BETHESDA, and thyroid malignancy histopathology. The data were considered significant if the p-value was <0.05. Diagnostic tests were based on receiver operating curve (ROC) analysis of FNAB (BETHESDA), USG (TI-RADS), and a combination of both in establishing a diagnosis of malignancy based on the histopathological examination results. In determining the cutoff point values, we assessed the point of intersection between sensitivity and specificity values. The cutoff point determined the values of FNAB (BETHESDA) and USG (TI-RADS) in establishing a diagnosis of malignancy based on the results of histopathological examination.
Results
The baseline characteristics of the research sample (Table 1), consisting of 47 patients with thyroid tumors, revealed the FNAB, USG, and histopathology examination findings.
| Characteristic | n (%) or mean (SD) |
| Age (years) | 47.93 ± 13.84 |
| Gender | |
| Male | 7 (14.9) |
| Female | 40 (85.1) |
| FNAB (BETHESDA) | |
| I | 3 (6.4) |
| II | 7 (14.9) |
| III | 3 (6.4) |
| IV | 16 (34.0) |
| V | 3 (6.4) |
| VI | 15 (31.9) |
| USG (TI-RADS) | |
| TR 1 | 1 (2.1) |
| TR 2 | 0 (0.0) |
| TR 3 | 9 (19.1) |
| TR 4A | 6 (12.8) |
| TR 4B | 21 (44.7) |
| TR 5 | 10 (21.3) |
| Histopathology | |
| Malignant | 41 (87.2) |
| Benign | 6 (12.8) |
The mean age of individuals with thyroid tumors was 47.93 years, with women comprising the majority (40, 85.1%). Based on FNAB examination results using the BETHESDA scoring system, the highest proportion of samples was classified as Grade IV, accounting for 16 (34.0%) samples, followed by Grade VI with 15 (31.9%) samples. Regarding USG examination results using the TI-RADS scoring system, most samples were in the TR 4B group, totaling 21 (44.7%). Based on histopathology examination (considered the gold standard), 41 (87.2%) samples showed malignancy.
The relationships between clinical characteristics and thyroid malignancy based on histopathological findings were examined (Table 2).
| Variable | Histopathology | p-value | |
| Malignant | Benign | ||
| (n=41) | (n=6) | ||
| Age (years) | 48.48 ± 14.10 | 44.16 ± 12.33 | 0.481* |
| Sex | |||
| Male | 6 (14.6) | 1 (16.7) | 1.000** |
| Female | 35 (85.4) | 5 (83.3) |
Notes: *Independent t-test; **Fisher exact test.
The mean age in the thyroid tumor group with malignant histopathology was higher at 48.48 years compared to the benign group at 44.16 years. However, this difference was not statistically significant in relation to thyroid malignancy based on histopathological findings (p>0.05). Additionally, women showed more prevalent thyroid malignancy based on histopathological findings. Similarly, no statistically significant gender difference was found concerning thyroid malignancy based on histopathological findings (p>0.05).
Table 3 and Figure 1 illustrate the diagnostic test results based on ROC curve analysis for FNAB (BETHESDA), USG (TI-RADS), and their combination in establishing a diagnosis of malignancy based on histopathological findings.
| Parameter | FNAB (BETHESDA) | USG (TI-RADS) | FNAB and USG |
| AUC | 0.835 | 0.843 | 0.756 |
| 95% CI | 0.698–0.927 | 0.708–0.933 | 0.609–0.869 |
| Cutoff | >3 | >4 | ≥1 |
| p-value | <0.001 | <0.001 | <0.001 |
| Accuracy (%) | 80.85 | 74.46 | 59.57 |
| Sensitivity (%) | 80.48 | 73.17 | 53.65 |
| Specificity (%) | 83.33 | 83.33 | 100 |
| PPV (%) | 97.05 | 96.8 | 100 |
| NPV (%) | 38.46 | 31.2 | 24 |
Note: NPV, negative predictive value; PPV, positive predictive value
Figure 1. ROC Curves for FNAB, USG Examination, and Combination of both in Assessing Diagnosis of Malignancy Based on Histopathological Examination Results.
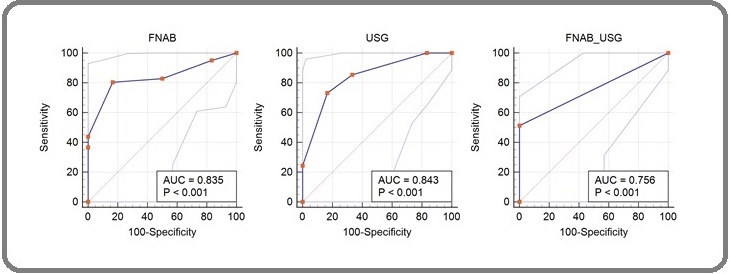
For FNAB (BETHESDA) examination in determining malignancy diagnosis, the cutoff point was above 3 (a minimum score of 4). For USG (TI-RADS) examination, the cutoff point was above 4a (a minimum score of 4b). The combined score of FNAB and USG examination was determined by merging both scores, where if the FNAB (BETHESDA) score was >3 and the USG (TI-RADS) score was >4a, then both test results were considered positive. Subsequently, an analysis was conducted to demonstrate the accuracy level based on the prediction model, yielding good results with area under curve (AUC) values of 0.835 (83.5%), 0.843 (84.3%), and 0.756 (75.6%) for FNAB (BETHESDA), USG (TI-RADS), and their combination, respectively.
Based on accuracy values, FNAB (BETHESDA) demonstrated better results at 80.85% compared to USG (TI-RADS) and their combination. Similarly, concerning sensitivity values, FNAB (BETHESDA) showed better results at 80.48% compared to USG (TI-RADS) and their combination. However, concerning specificity values, the combination of FNAB (BETHESDA) and USG (TI-RADS) examinations exhibited the best results at 100.0% compared to individual examinations.
Discussion
The high proportion of patients in this study diagnosed with malignancy and advanced stages was possible because the patients admitted to our institution are mostly referred from primary and secondary health facilities. Patients with lower tumor gradings can be treated at health facilities in their regions. Rahwamati et al. explained that one of the possible delays in patients attending health services is the tendency of Indonesian people to go to health facilities only when the tumor has reached a significant size or complex condition, along with the lack of public knowledge regarding the early detection of malignant diseases other than breast cancer [11].
One strategy that is still commonly used is determining the risk profile based on patient characteristics. Moon et al. showed that thyroid nodules can be associated with gender (women are more at risk than men), advanced age, central obesity, hypertension, diabetes, and a history of fatty liver [12]. This is comparable to the profile of patient characteristics in our study, where based on mean age, the thyroid tumor group with malignant histopathology was older (48.48 years) than the benign group (44.16 years), but this result was not significant (p>0.05). Furthermore, our study found that thyroid malignancies based on histopathological features were more common in women (83.3%) than men (16.7%), although based on analysis using the Fisher exact test, this difference was not statistically significant (p>0.05).
The etiology of thyroid carcinoma remains uncertain [13]. Environmental factors, genetics, and autoimmunity are suspected to play a role. The incidence of FTC and possible ATC is high in areas with iodine deficiency. Iodine deficiency leads to chronic TSH stimulation due to low thyroid hormone synthesis, resulting in carcinoma formation [14, 15]. Thyroid carcinoma is estimated to account for 5–10% of all thyroid nodules in humans [2]. Thyroid nodules are a malignancy often found in Indonesia. In determining staging and prognostic value and treatment planning, standardization of thyroid nodule case reporting is needed. The latest developments in thyroid nodule examination focus on two main types of staging modalities: TI-RADS and BETHESDA. The TI-RADS system is a radiological reporting standard, whereas BETHESDA is the standard used in cytological examinations. This study aimed to assess the accuracy of the combination of TI-RADS and BETHESDA in the histopathology of thyroid malignancies so that it can be a reference when consideration is needed to provide the most effective and efficient examination facilities for assessing thyroid malignancies, especially in areas with limited facilities.
Thyroid nodules are generally asymptomatic, and most patients diagnosed with thyroid malignancy are not critical when brought to the hospital. This is because most asymptomatic thyroid nodules are benign, with thyroid hormone secretion levels still within normal limits, and the risk of developing cancer only ranges from 0.45% to 13% [16]. Only patients with nodules and a certain level of risk are expected to undergo diagnostic procedures, but with the development of technology and examination modalities such as ultrasound and FNAB, thyroid nodule malignancy can be detected as early as possible so that appropriate management can be started earlier.
Studies have defined thyroid nodules as distinctive lesions within the thyroid gland that present radiological differences from the surrounding thyroid parenchyma. These nodules can be solitary or multiple, solid or cystic, and functional or non-functional [17]. Therefore, ultrasound examination is considered reliable for identifying cases of thyroid nodules, but it has limitations in accurately distinguishing between benign and malignant tumors. Hence, a combination of ultrasound and FNAB is needed to rule out the possibility of malignancy and prevent total thyroid removal procedures without confirmation from both examinations.
Our study aimed to assess the accuracy of TI-RADS and BETHESDA in evaluating the malignancy of thyroid nodules to provide recommendations for minimal effective examinations that can be used in areas with limited healthcare facilities. The good results obtained indicated that both single examinations, either USG or FNAB, and their combination can be relied on to ensure the diagnosis of thyroid nodules.
Based on the accuracy and sensitivity values, FNAB (BETHESDA) statistically demonstrated superiority (accuracy 80.85% and sensitivity 80.48%) compared to USG (TI-RADS) and their combination. However, concerning specificity values, the combination of FNAB (BETHESDA) and USG (TI-RADS) examinations showed the best results compared to individual examinations (100%). This indicates that, for the specificity of diagnosing thyroid nodules, the combination of TI-RADS and BETHESDA remains necessary.
The limitation of this study is that similar research is needed with a larger sample size. Studies should also be carried out in multicenter hospitals with minimal examination modalities of ultrasound and FNAB to improve the statistical analysis in assessing the accuracy of diagnostic examinations.
In conclusions, these findings suggest that while FNAB (BETHESDA) is accurate and sensitive, the integration of both methods enhances specificity, making it a valuable approach for clinical decision-making. This could lead to improved diagnostic accuracy and better patient outcomes, as integrating both methods may provide a more comprehensive assessment of thyroid nodules. Furthermore, exploring the synergistic effects of these methods could lead to improved patient outcomes and reduced unnecessary interventions.
Acknowledgements
The researchers would like to express their sincere gratitude to the Dr Wahidin Sudirohusodo Hospital and Faculty of Medicine at Hasanuddin University in Makassar, Indonesia, for their generous support of this research.
Contributors
EHC: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. SAS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Software, Validation, Visualization, Writing – original draft. NS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. FH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. MF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing.
Competing interests
No competing interests were reported.
Ethics approval
The study was approved by the Research Ethics Committee of the Faculty of Medicine Universitas Hasanuddin, Makassar, Indonesia, number: (No: 293/UN4.6.4.5.31/PP36/2024 with protocol number: UH24040265 on May 2, 2024. We promised that the participants’ data were anonymized or maintained with confidentiality, the rights or interests of participants were not invaded, and informed consent was taken from all individual participants.
Data availability statement
Data is accessible upon justifiable request.
References
- The Thyroid And Its Diseases - A Comprehensive Guide For The Clinician Corin Badiu M. D.. Acta Endocrinologica (Bucharest).2018;14(4). CrossRef
- Pathogenesis of Thyroid Carcinoma. In: Vitti P HL (ed.) Thyroid Diseases Pathogenesis, Diagnosis, and Treatment. 1st ed Santoro M CF . Springer International Publishing.2018.
- The Bethesda System for Reporting Thyroid Cytopathology: A Cytohistological Study Anand B, Ramdas A, Ambroise MM , Kumar NP . Journal of Thyroid Research.2020;2020. CrossRef
- Genomic Profiling of Thyroid Nodules: Current Role for ThyroSeq Next-Generation Sequencing on Clinical Decision-Making Kargi AY , Bustamante MP , Gulec S. Molecular Imaging and Radionuclide Therapy.2017;26(Suppl 1). CrossRef
- Comparison between Sonographic Features and Fine Needle Aspiration Cytology with Histopathology in the Diagnosis of Solitary Thyroid Nodule De D, Dutta S, Tarafdar S, Kar SS , Das U, Basu K, Mukhopadhyay P, Ghosh S. Indian Journal of Endocrinology and Metabolism.2020;24(4). CrossRef
- Classification of thyroid fine-needle aspiration cytology into Bethesda categories: An institutional experience and review of the literature Alshaikh S, Harb Z, Aljufairi E, Almahari SA . CytoJournal.2018;15. CrossRef
- Thyroid Imaging Reporting and Data System (TI-RADS): A User's Guide Tessler FN , Middleton WD , Grant EG . Radiology.2018;287(1). CrossRef
- A novel TIRADS of US classification Zhuang Y, Li C, Hua Z, Chen K, Lin JL . Biomedical Engineering Online.2018;17(1). CrossRef
- Risk for malignancy of thyroid nodules: Comparative study between TIRADS and US based classification system Ashamallah G, EL-Adalany M. The Egyptian Journal of Radiology and Nuclear Medicine.2016;47. CrossRef
- Correlation of Thyroid Fine Needle Aspiration Biopsy With Histopathological Results Durgun C. Cureus.2023;15(5). CrossRef
- In Vitro Evaluation of Cytotoxicity Effect of Ihau Fruit Extract (Dimocarpus longan var. Malesianus Leenh.) on MCF-7 Breast Cancer Cell Line Sarita I, Dyanti G, Widyanto R, Maulidiana A, Nabila W, Purwestri R. Indonesian Journal of Human Nutrition.2023;10. CrossRef
- Prevalence of thyroid nodules and their associated clinical parameters: a large-scale, multicenter-based health checkup study Moon JH , Hyun MK , Lee JY , Shim JI , Kim TH , Choi HS , Ahn HY , et al . The Korean Journal of Internal Medicine.2018;33(4). CrossRef
- Thyroid carcinoma: epidemiology, histology, and diagnosis Shah JP . Clinical Advances in Hematology & Oncology: H&O.2015;13(4 Suppl 4).
- 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer Haugen BR , Alexander EK , Bible KC , Doherty GM , Mandel SJ , Nikiforov YE , Pacini F, et al . Thyroid: Official Journal of the American Thyroid Association.2016;26(1). CrossRef
- Diagnosis and treatment of patients with thyroid cancer Nguyen QT , Lee EJ , Huang MG , Park YI , Khullar A, Plodkowski RA . American Health & Drug Benefits.2015;8(1).
- Prevalence of Thyroid Nodules and Associated Clinical Characteristics: Findings from a Large Sample of People Undergoing Health Checkups at a University Hospital in Vietnam Tran NQ , Le BH , Hoang CK , Nguyen H, Thai TT . Risk Management and Healthcare Policy.2023;16. CrossRef
- Management of Thyroid Nodules Uludag M, Unlu MT , Kostek M, Aygun N, Caliskan O, Ozel A, Isgor A. Sisli Etfal Hastanesi Tip Bulteni.2023;57(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2025
Author Details