Breast Cancer Awareness, Screening Practices, Barriers, and Educational Interventions in Middle Eastern Countries: Challenges and Successes
Download
Abstract
Objective: This review explores breast cancer awareness, knowledge, and screening practices among women in Gulf andMiddle Eastern countries, highlighting disparities and challenges within the region.
Methods: A systematic literature review was conducted using databases like PubMed, Scopus, and Google Scholar to identify English-language studies (2015 onward) on breast cancer awareness, knowledge, and screening practices among women in Gulf and Middle Eastern countries. Data from eligible studies were independently extracted by two reviewers, and a weighted average formula was applied to synthesize findings, ensuring greater influence from larger sample sizes while minimizing redundancy across countries.
Results: By synthesizing findings from 25 studies, the review identifies significant variations in breast cancer awareness levels, with 30% of populations exhibiting high awareness, 45% moderate awareness, and 25% low awareness. A weighted average analysis reveals gaps between awareness and practices of screening methods: while 75% of women were aware of breast self-examination (BSE), only 45% practiced it; similarly, awareness of mammography stood at 60%, but practice levels were as low as 35%. Key barriers to timely medical help-seeking include emotional (65%), informational (50%), and financial (40%) factors, underscoring the role of cultural stigmas, logistical challenges, and limited healthcare access. Educational interventions demonstrated success in bridging awareness gaps, increasing awareness by 85% and improving help-seeking behavior by 70%. Effective initiatives include school-based health education, digital platforms, and community outreach. However, challenges persist in addressing cultural and psychological barriers and ensuring equitable healthcare access.
Conclusion: Lessons from developed countries emphasize the value of integrated public health campaigns, proactive healthcare engagement, and advanced technology in improving breast cancer outcomes. The review concludes with actionable recommendations to enhance awareness, screening practices, and healthcare systems across the Gulf and Middle East, paving the way for earlier detection and better survival rates.
Introduction
Breast cancer is the most commonly diagnosed cancer among women worldwide, representing a significant public health concern [1]. Early detection through heightened awareness and regular screening is critical for improving survival rates and reducing mortality. In many regions, comprehensive public health campaigns and structured screening programs have significantly improved early detection rates [2- 5]. However, in Middle Eastern countries, disparities in breast cancer awareness and screening practices persist, driven by a combination of cultural, educational, social, and healthcare-related barriers [6].
Cultural and social norms in Middle Eastern countries play a pivotal role in shaping health behaviors and attitudes toward breast cancer screening. Modesty, fear, and fatalism are deeply ingrained in many communities, leading to reluctance in discussing and participating in breast health practices [7]. Social stigmas surrounding cancer, compounded by its taboo nature, further exacerbate these barriers. The limited public discourse on breast cancer translates into low awareness and knowledge levels regarding early detection and available screening methods [8-9].
Educational and informational gaps, along with healthcare access challenges, also significantly hinder breast cancer screening rates in the region. Many women have limited knowledge about breast cancer symptoms, risk factors, and the importance of early detection [10]. Educational initiatives, although implemented, often fail to address the population effectively or reach underserved groups [11-13]. Financial constraints, lack of transportation, and family responsibilities further restrict women’s access to healthcare services [14-15]. Moreover, healthcare systems in certain Middle Eastern countries lack adequate resources to support large-scale screening programs and follow-up care.
This literature review investigated the current state of breast cancer awareness, knowledge, and screening practices among women in Gulf and Middle Eastern countries, highlighting cultural, social, and logistical barriers to early detection. By examining these challenges and evaluating educational interventions, this study aimed to provide evidence-based recommendations for improving breast cancer awareness and screening uptake in the region.
Methods
This literature review analyzed recent studies focusing on breast cancer awareness, knowledge, and screening practices among women in Gulf and Middle Eastern countries, including Oman, Bahrain, Kuwait, Qatar, the Kingdom of Saudi Arabia (KSA), the United Arab Emirates (UAE), Jordan, Iran, Turkey, Syria, Lebanon, Palestine, and Egypt. Inclusion criteria for the review were studies published since January 2015, written in English, involving national samples of female participants, and addressing breast cancer awareness, knowledge, attitudes,practices, or screening behaviors.
A comprehensive literature search was conducted using databases such as PubMed, Google Scholar, and Scopus. Search keywords included “breast cancer awareness,” “breast cancer knowledge,” “breast cancer screening,” “Gulf countries,” and the names of the target countries (e.g., Oman, Bahrain, Kuwait, Qatar, the KSA, the UAE, Jordan, Iran, Turkey, Syria, Lebanon, Palestine, and Egypt). Additional articles were identified through manual searches of reference lists from relevant studies to ensure inclusiveness.
Data abstraction was performed using a standardized form by two independent researchers to capture critical information from each study. Extracted data included author (s) and year of publication, study location, design and methodology, sample size, data collection instruments, and key findings related to breast cancer awareness, knowledge, and screening practices. The abstracted data reliability between the two independent researchers was around 96%. Discrepancies between the two researchers were then discussed and an agreement was made.
The weighted average was calculated to synthesize findings from multiple studies, ensuring a balanced representation of awareness and screening practices across different countries. The calculation was performed using the following formula:
Weighted Average= ∑(Percentage×Sample Size)/ Total Sample Size across all studies Where:
• Percentage represents the reported prevalence or awareness level from each study.
• Sample Size is the number of participants in that specific study.
• Total Sample Size is the sum of all individual study sample sizes
This approach ensured that findings from studies with larger sample sizes carried greater influence, providing a more representative overall analysis of population- weighted proportions for breast cancer awareness and practices in the region .While this method provides an aggregated estimate, we acknowledge that it treats all studies equally, regardless of variations in participant sample sizes. To address this limitation, we ensured that only distinct studies from different population groups were included to minimize redundancy or overrepresentation from any single country.
Results
The literature review encompasses 25 studies investigating breast cancer awareness, knowledge, and screening practices among women in Gulf and Middle Eastern countries. These studies are distributed across several countries: Oman [8-10], Bahrain [16-17], Kuwait [18-19], Qatar [20], KSA [21-22], UAE [13, 23-24], Jordan [25-26], Iran [27-28], Turkey [29], Syria [30-31], Lebanon [14], Palestine [15, 32], and Egypt [11-12].
The Majority of studies (n=17) were cross-sectional, offering snapshots of breast cancer awareness and practices, such as those by Al-Ismaili et al. (2020) and Al-Azri et al. (2021) in Oman and Elmaghraby et al. (2023) in KSA. Two qualitative studies in Kuwait [18-19] used focus groups and interviews to explore perceptions. An interventional randomized controlled trial by Al-Hosni et al. (2023) in Oman assessed the impact of educational programs on adolescents.
A mixed-methods study by Elgammal (2023) in Bahrain evaluated health awareness campaigns’ effectiveness. The systematic review by AlRajhi et al. (2023) in KSA synthesized findings on breast cancer awareness, while Al Hosani et al. (2022) conducted a descriptive cross-sectional study in the UAE on breast cancer knowledge and self-diagnostic skills.
Knowledge of Breast Cancer
The levels of breast cancer knowledge in the Gulf and Middle Eastern countries vary significantly across the region (Figure 1).
Figure 1. The Levels of Breast Cancer Knowledge in the Gulf and Middle Eastern Countries A Weighted Average was Used. Weighted Average= ∑(Percentage×Sample Size)/ Total Sample Size. High Awareness (30%): Represents populations with excellent general knowledge about breast cancer. Moderate Awareness (45%): Reflects groups with good awareness but noticeable gaps or misconceptions about specific aspects, such as risk factors or screening methods. Low Awareness (25%): Includes populations with poor knowledge or significant educational deficiencies.
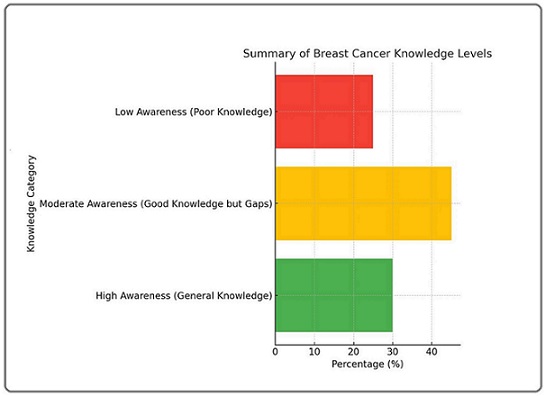
The awareness levels (high: 30%, moderate: 45%, low: 25%) represent population-weighted proportions, calculated by considering the sample sizes of each study to ensure an accurate regional estimate where the studies reported different awareness levels with varying sample sizes, the final proportion accounts for each study’s contribution relative to its participant count. High awareness (30%) represents populations with excellent general knowledge about breast cancer, such as Jordan, where 99.5% of women had heard of breast cancer [25]. Moderate awareness (45%) includes groups with good overall knowledge but noticeable gaps, such as Oman, where 60.5% of female teachers demonstrated good knowledge [8], and Qatar, where 69% of women recognized warning signs but lacked knowledge of risk factors [20]. Low awareness (25%) reflects significant educational deficiencies, as seen in Bahrain, where 63.25% of university students had poor knowledge of breast self-examination [17], and the UAE, where only 6% of women had excellent knowledge [24].
Several countries demonstrated specific challenges. For instance, Palestine reported only 38.4% of women with good knowledge of risk factors [15], while in Lebanon, high recognition of carcinogens like smoking (97.5%) [14]. Misconceptions about risk factors persists in Jordan [26], and in Oman only 9% of female teachers showed excellent knowledge of risk factors [8]. The Kingdom of Saudi Arabia showed a low awareness (66.3%) of breast cancer risk factors [21], and in Turkey, 41.2% of women recognized risk factors like smoking and family history [29]. Syria showed negative correlations between awareness and factors like smoking and marital status [30]. While, family history was frequently recognized as a risk factor in Palestine, other factors were less understood [32]. Also, the psychological and informational barriers influenced the studies participants knowledge of breast cancer. In Iran, self-efficacy and motivation were linked to awareness levels [27]. These findings underscore the need for targeted educational programs to address gaps and misconceptions across the region.
Screening Methods
Awareness and practice of breast cancer screening methods, including Breast Self-Examination (BSE), clinical breast examination (CBE), and mammography, showed a significant variation across the Gulf and Middle Eastern countries (Figure 2).
Figure 2. The Awareness and Practice Levels of Breast Cancer Screening Methods in the Gulf and Middle Eastern Countries A Weighted Average was Used. Weighted Average= ∑(Percentage×Sample Size)/ Total Sample Size.• Awareness of Breast Self-Examination (BSE): 75%. • Practice of Breast Self-Examination (BSE): 45%. • Awareness of Mammography: 60%. • Practice of Mammography: 35% .
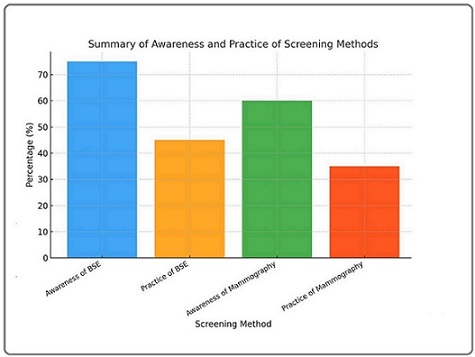
Awareness of BSE is relatively high (75%) compared to its practice (45%), indicating that knowledge is present but not consistently translated into action. This lower adoption of the BSE practice levels may highlight gaps in motivation, confidence, or understanding. Awareness of mammography is moderate (60%), demonstrating a room for improvement through targeted outreach and educational programs. The practice of mammography remains the lowest (35%), which may reflect the presence of barriers such as limited access, insufficient awareness campaigns, and cultural or motivational challenges.
In Jordan, 90.5% of women were aware of BSE, but only 52.75% practiced it [25], revealing a considerable gap. Similarly, in Oman, 57% of female teachers practiced BSE, which was positively linked to breast cancer knowledge [8]. Bahrain demonstrated that only 56.03% of university students practiced BSE, despite some knowledge of the method [17]. In the UAE, 46% of women practiced BSE, highlighting a need for further educational initiatives [23]. In KSA, 59.4% of women did not perform BSE regularly, emphasizing the need for motivational strategies [21]. Syria showed even lower confidence, with only 16.4% of women expressing confidence in detecting breast changes [31].
Regarding mammography, awareness varies. In KSA, 67.5% of women were aware of mammography, but Elmaghraby et al. (2023) noted that follow-through was insufficient. Oman showed relatively high awareness levels, with 56.1% of female teachers demonstrating excellent knowledge of screening methods [8]. However, Turkey had lower awareness, with only 23.3% of women aware of mammography and 19% aware of ultrasonography [29]. In Iran, 38.2% of women had a mammogram in the last 24 months, suggesting moderate awareness but barriers to access [27]. These findings underline the need for region-specific interventions to improve awareness and practice of breast cancer screening methods.
Barriers to Seeking Medical
Help Barriers to seeking medical help significantly hinder timely care in the Gulf and Middle Eastern regions, categorized as emotional, financial, and informational barriers (Figure 3).
Figure 3. Barriers to Seeking Medical Help A Weighted Average Was Used. Weighted Average= ∑(Percentage×Sample Size)/ Total Sample Size. • Emotional Barriers (65%): Fear, anxiety, and worry about diagnosis were the most sig- nificant barriers, as highlighted in multiple studies across regions such as Oman, Bahrain, and Saudi Arabia. • Finan- cial Barriers (40%): Costs and accessibility issues were key factors, notably in Jordan and other areas with limited healthcare affordability. • Informational Barriers (50%): Lack of knowledge, misconceptions, and not knowing how to perform Breast Self-Examinations (BSE) were frequently mentioned, particularly in Palestine and Egypt.
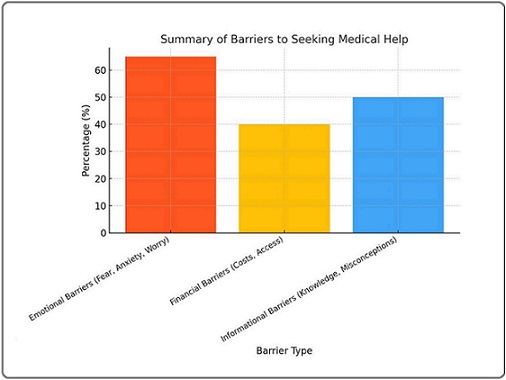
Emotional barriers (65%) such as fear, anxiety, and worry about diagnosis were the most prominent, particularly in Oman (68.9%), where misconceptions like fatalism further delayed help-seeking behaviors [9, 21]. Financial barriers (40%) like costs and accessibility issues were critical factors in Jordan, where 57% cited these as obstacles [14]. Informational barriers (50%), such as lack of knowledge and misconceptions about breast self-examinations (BSE), were notably prevalent in Palestine and Egypt [12, 32].
Delays in help-seeking behaviors were reported across multiple regions. In Oman, 66.4% sought medical help within a month of noticing symptoms despite high awareness [9]. In Qatar, delays were tied to appointment difficulties and fear of diagnosis, despite 94% attending screenings when directly invited [20]. In Bahrain, anxiety, shyness, and fatalism were key barriers to mammograms [16]. In Palestine, only 4.1% practiced BSE due to lack of knowledge and absence of breast problems [32]. Egypt similarly highlighted barriers in knowledge and confidence, with only 22.9% practicing BSE correctly [12].
Educational Interventions
Educational interventions have demonstrated varied success in improving breast cancer awareness and practices across the Gulf and Middle Eastern countries (Figure 4).
Figure 4. The Outcomes of Educational Interventions Aimed at Improving Breast Cancer Awareness and Practices A Weighted Average was Used. Weighted Average= ∑(Percentage×Sample Size)/ Total Sample Size. • Increased Awareness (85%): Educational programs significantly raised awareness about breast cancer risk factors and symptoms across multiple countries. • Improved Help-Seeking Behavior (70%): Interventions reduced barriers to seeking medical help, particularly in Oman and Jordan. • Reduced Misconceptions (60%): Targeted efforts helped correct false beliefs about breast cancer, such as its causes and risk factors, as seen in Kuwait. • Positive Screening Attitudes (75%): Campaigns promoted favorable views on breast cancer screening, with social media playing a crucial role in the UAE.
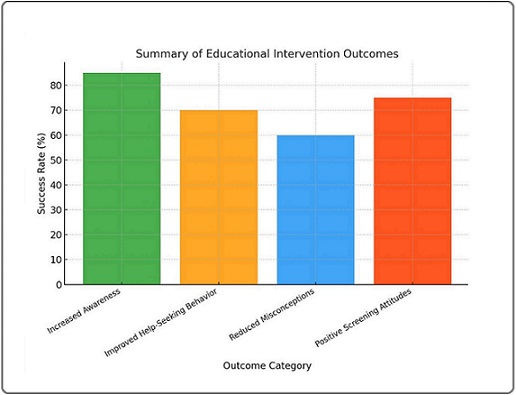
These programs significantly increased awareness (85%), improved help-seeking behavior (70%), reduced misconceptions (60%), and fostered positive screening attitudes (75%). In Jordan, general awareness of breast cancer reached 99.5% among adult women, indicating the effectiveness of such interventions [25]. In Oman, a one-hour educational session enhanced students’ recognition of risk factors and reduced barriers to seeking help [9]. Iran highlighted the importance of implementing educational programs in schools to encourage early detection practices [28].
In Oman, intervention groups exhibited significant improvements in both awareness and help-seeking behaviors compared to control groups [10]. In the UAE, positive attitudes toward screening were linked to information from health professionals and social media campaigns [13]. In KSA, the need for robust educational initiatives to enhance awareness and promote early detection was emphasized [22]. Kuwait addressed misconceptions, such as beliefs linking breast cancer to breastfeeding or genetics, which hindered screening uptake [18]. Similarly, Turkey demonstrated that education and marital status significantly influenced awareness levels, highlighting the importance of targeted interventions [29].
Discussion
This review highlighted significant variations in breast cancer awareness, knowledge, and screening practices across the Gulf and Middle Eastern countries, emphasizing the multifaceted challenges influencing outcomes [2, 10, 20]. The studies included in this review varied in design, with the majority being cross-sectional providing a snapshot of breast cancer awareness and screening practices. While these studies offer broad insights into prevalence and knowledge levels, they do not establish causality or long-term trends. In contrast, qualitative studies provided in-depth perspectives on cultural and psychological barriers, helping contextualize quantitative findings but limiting generalizability due to smaller sample sizes [2, 33].
Interventional studies demonstrated the effectiveness of educational programs, highlighting potential strategies for improving awareness and screening uptake. Additionally, systematic reviews synthesized multiple studies, enhancing the robustness of findings but potentially introducing publication bias [34-36].
The heterogeneity in study designs means that comparisons across studies must be interpreted with caution. While weighted averages were used to summarize numerical findings, differences in methodologies, sample populations, and data collection tools could introduce inconsistencies. To account for this, we ensured that only studies with clear methodologies and representative populations were included in the synthesis. Future research should prioritize longitudinal studies and standardized methodologies to better assess trends over time and improve comparability across regions.
Developed countries utilize long-term cohort studies to monitor how awareness campaigns, policy changes, and screening accessibility impact breast cancer detection rates over years. Similar approaches in Middle Eastern countries could identify which interventions have a lasting effect and which require modifications [34-36].
Larger studies, such as those conducted in Qatar, leveraged robust healthcare infrastructure to collect comprehensive data, while smaller qualitative studies provided nuanced insights into socio-cultural factors affecting breast cancer awareness and behaviors [19]. Compared to developed countries, where well-established longitudinal studies are more common, the reliance on cross-sectional research in the Gulf and Middle Eastern countries limits the ability to track long-term trends and evaluate the sustained impact of interventions [3].
In contrast to developed countries, where there is a widespread public health campaigns and school-based education programs ensuring a high awareness of breast cancer across their diverse populations [6], in the Gulf and Middle Eastern countries showed a variations in general breast cancer awareness which reflect a disparity in public health education and access to information across the region. High awareness levels, such as those seen in Jordan (99.5%), are indicative of successful, targeted initiatives. However, low awareness in countries like Bahrain and the UAE underscores significant deficiencies in public health education [2, 8, 17].
Persistent misconceptions about risk factors in the Gulf and Middle Eastern countries, even in regions with moderate awareness levels like Oman and Qatar, highlight the need for culturally tailored and ongoing educational efforts [20]. By contrast, developed countries typically experience lower rates of misconceptions due to comprehensive education integrated into healthcare services and community programs [3]. Psychological and motivational factors, as seen in Iran, further influence awareness and behavior, demonstrating the need for interventions addressing both knowledge and emotional readiness, a strategy effectively utilized in Western nations [1, 27].
The disparity between awareness and practice of screening methods, including BSE, CBE, and mammography, is a recurring issue. While awareness of BSE is relatively high (75%), its practice (45%) is hindered by cultural stigmas, low confidence, and motivational challenges [21]. Awareness of mammography (60%) also fails to translate into high practice levels (35%), reflecting systemic barriers such as accessibility issues and inadequate public health campaigns [2, 22, 29].
Comparatively, developed countries exhibit higher rates of both awareness and practice due to well-structured healthcare systems that encourage preventive care and routine screenings through proactive engagement by healthcare providers [4]. Regular reminders, incentives for screenings, and easily accessible facilities in Western nations ensure higher compliance rates, whereas logistical barriers and limited healthcare infrastructure in the Gulf and Middle Eastern countries impede participation [6].
Emotional, financial, and informational barriers significantly delay medical help-seeking behaviors in the Gulf and Middle East. Emotional barriers, such as fear and anxiety about diagnosis, are prevalent in countries like Oman and Bahrain, where cultural norms often discourage open discussions about health [9, 16]. The study of Moey et al. (2022) found that Muslim women religious and cultural beliefs of exposing their sensitive body organ like breast to a male healthcare provider or discussing their breast health concerns are one of the major barriers to breast cancer screening. Such a misperceived concern needs to be addressed by a community action groups that include religious representatives, Tribes masters and politicians [33].
In many Middle Eastern societies, religious figures and tribal leaders play a crucial role in shaping health behaviors. Integrating breast cancer awareness messages into Friday sermons, religious gatherings, and community events can help normalize discussions around screening while addressing fatalistic beliefs. Utilizing female health ambassadors, particularly those from within the community (e.g., teachers, nurses, breast cancer survivors), can reduce modesty-related hesitations and encourage open discussions [33].
Public health campaigns should emphasize that early detection aligns with Islamic teachings on health preservation and that screening procedures can be done in women-only environments, reducing concerns about modesty. In societies where family members influence women’s healthcare decisions, educating husbands and sons about the importance of screening can lead to increased support for timely medical check-ups [34-36]. In developed countries, emotional barriers are mitigated through integrated psychological support in healthcare settings, coupled with public health campaigns that normalize breast cancer discussions [1]. Financial constraints and limited healthcare access, as seen in Jordan and Palestine, further restrict participation in screening programs, while developed nations with comprehensive health insurance systems ensure equitable access to preventive care [14, 32].
Informational barriers, such as misconceptions and lack of knowledge about BSE or mammography, remain widespread in the Gulf and Middle Eastern countries. In contrast, developed countries invest significantly in health education, leveraging digital tools and mass media to promote accurate information dissemination [2, 3].
Educational interventions demonstrate potential in bridging awareness and practice gaps but require sustained efforts for long-term impact. In Oman, short, targeted sessions significantly improved recognition of breast cancer risk factors among adolescents, illustrating the value of focused interventions [10].
Integrating health education into school curricula, as recommended in Iran, could provide scalable and sustainable improvements [28]. The use of digital tools, such as social media campaigns in the UAE, highlights the increasing role of technology in public health education [13]. However, misconceptions and barriers persist, highlighting the need for comprehensive and culturally sensitive strategies. By comparison, developed countries have institutionalized breast cancer education within schools, healthcare systems, and community outreach programs, ensuring consistent and widespread dissemination of accurate information [6]. Additionally, modern technology and professional networks are effectively leveraged to maintain high levels of awareness and promote regular screening practices in developed countries [1, 2].
Though the researchers did a comprehensive literature search and review through the primary and secondary sources, this paper has a couple of limitations. This study included studies that were published since January 2015. Also, it relied on a national sample of female participants studies. Moreover, the literature review search was from selected bibliographical databases (PubMed, Google Scholar, and Scopus). Beside these limitations, the majority of retrieved literature were cross sectional in nature, adopted different sampling strategies and discussed multiple variables or adopted different study designs such as the qualitative design. These limitations altogether could affect the generalizability of this paper results. Accordingly, the research team suggests to interpret this study findings with consideration to the above-mentioned limitations.
This review included only studies published in English, which may have led to the exclusion of relevant research published in Arabic, Farsi, Turkish, or other regional languages. As a result, valuable insights from non-English sources might not have been incorporated, potentially limiting the comprehensiveness of our findings. To mitigate this limitation, we ensured that studies covered diverse geographic locations and cross-referenced findings from multiple sources. Future research should consider systematic reviews incorporating multilingual studies or collaborations with regional researchers to capture a broader spectrum of evidence
To improve breast cancer awareness and screening practices in the Gulf and Middle Eastern countries, a multifaceted approach involving health ministries, health organizations, governments, community leaders, and researchers is essential. Health ministries should develop comprehensive national strategies that integrate breast cancer awareness into broader public health initiatives, enhance public health education through multimedia campaigns, and improve healthcare access by investing in infrastructure and providing subsidies for screening services. Health organizations need to provide training and resources for healthcare providers, support community- based interventions, and conduct regular evaluations to refine and adapt their programs.
Governments are advised to increase their funding for breast cancer research and preventive programs, enact supportive policies ensuring health insurance coverage for screenings, and integrate health education into school curricula to build a foundation of knowledge from a young age. Public-private partnerships can also play a crucial role in leveraging resources and expertise. Community leaders including politician, healthcare administrators, religious representatives and tribes masters are pivotal in advocating for health initiatives, addressing cultural barriers, and facilitating access to screening and treatment resources within their communities. Their influence can help dispel myths and encourage proactive health behaviors.
Researchers must focus on local contexts to understand the specific factors affecting breast cancer awareness and screening practices. They should develop and pilot tailored interventions, evaluate their effectiveness, and collaborate across disciplines to ensure practical application of their findings. By engaging with communities and stakeholders, researchers can ensure their work addresses real-world needs. Operationally, it is crucial to engage all relevant stakeholders, secure necessary funding, and establish robust monitoring and evaluation frameworks to track progress and continuously improve breast cancer awareness and screening programs. Multi-year follow-ups on participants who have undergone breast cancer education programs can help determine whether improvements in awareness translate into sustained behavior changes [1-3].
Platforms like WhatsApp, Instagram, and Facebook are widely used across the Middle East. Targeted digital campaigns such as short awareness videos in Arabic, Instagram Live sessions with female doctors, and WhatsApp health groups can facilitate widespread, culturally appropriate education [34-39]. AI-driven health chatbots tailored for Arabic, Persian, and Turkish speakers can provide private, anonymous responses to common concerns about screening, reducing embarrassment in asking sensitive questions [34-36].
Collaboration with female social media influencers especially hijabi influencers and mothers with strong followings can destigmatize breast cancer discussions by framing them as part of women’s health and family well-being. Developing mobile-friendly, interactive breast cancer awareness courses in local dialects can enhance access to information for women in rural or conservative communities, where traditional in-person education might not be feasible [34-37].
Recommendation and Clinical Implication
Priority 1: High-Feasibility, High-Impact Strategies (Short-Term Implementation, ≤2 Years).
Integrating breast cancer awareness into secondary school curricula is a crucial step toward early knowledge acquisition, ensuring that young individuals develop a foundational understanding of the disease before cultural barriers take root. Community-led awareness campaigns further enhance outreach by training local female health educators, breast cancer survivors, and religious figures to conduct culturally sensitive educational sessions in mosques, community centers, and women’s groups. These initiatives increase accessibility and foster trust within conservative communities. Additionally, leveraging social media and digital health tools, such as Instagram, WhatsApp, and AI-driven chatbots, allows for the dissemination of breast cancer information in Arabic, Farsi, and Turkish. This digital approach offers a cost-effective method to reach women in conservative settings where traditional healthcare access may be limited.
Priority 2: Mid-Term Strategies (2–5 Years, Requiring Policy Support)
Mandating workplace breast cancer screenings is a mid-term strategy aimed at normalizing preventive healthcare by requiring annual employer-sponsored screenings for women working in both the public and private sectors. This ensures a structured and systematic approach to early detection. Additionally, integrating clinical breast exams (CBE) and mammograms into routine primary healthcare visits promotes sustained participation in screening programs. By embedding breast cancer prevention into primary care services, women are more likely to undergo regular screenings without the need for additional appointments, reducing logistical and psychological barriers.
Priority 3: Long-Term Structural and Policy Reforms (5+ Years)
Establishing national breast cancer screening programs with government-subsidized mobile mammography units is essential for ensuring equitable healthcare access, particularly for women in rural and underserved areas. Expanding insurance coverage for mammograms and providing government subsidies for low-income populations further reduces financial barriers, making screenings more accessible to all socioeconomic groups.
Additionally, conducting longitudinal research and data collection on awareness campaigns and screening interventions enables evidence-based policymaking, ensuring that future strategies are data-driven and continuously optimized for effectiveness.
Stakeholder Collaboration for Effective Implementation
Health ministries and governments play a critical role in funding national awareness programs, integrating breast cancer education into schools, mandating screening policies in government healthcare facilities and workplaces, subsidizing screenings for uninsured and low-income populations, and fostering public-private partnerships to expand mobile screening services. Non-governmental organizations (NGOs) and advocacy groups can enhance outreach by organizing community-based programs targeting underserved populations, funding and distributing free multilingual educational materials, training female health ambassadors to lead culturally sensitive awareness sessions, and collaborating with social media influencers to amplify awareness. Community leaders, including religious figures, tribal leaders, and social influencers, also contribute by promoting health-positive messaging through sermons, community meetings, and cultural events, endorsing local awareness initiatives to reduce stigma and misconceptions, and creating safe spaces for women to discuss breast cancer prevention. Through coordinated efforts among these stakeholders, breast cancer awareness and early detection efforts can be significantly strengthened across diverse communities.
In conclusion, this review underscores the considerable disparities in breast cancer awareness, knowledge, and screening practices across the Gulf and Middle Eastern countries, emphasizing the need for multifaceted strategies to address these gaps. While some countries have achieved high awareness levels through targeted public health campaigns and educational initiatives, others continue to face significant challenges due to cultural stigmas, financial constraints, and limited healthcare infrastructure. The disparity between awareness and actual practice of screening methods, such as BSE and mammography, highlights the critical need to translate knowledge into actionable behaviors. Emotional and informational barriers further compound these issues, underscoring the importance of culturally sensitive and accessible interventions to encourage early detection and improve health outcomes.
By leveraging lessons from developed countries, the Gulf and Middle Eastern nations can adopt more integrated approaches to breast cancer education and screening. These include incorporating health education into school curricula, expanding access to affordable healthcare services, and utilizing digital platforms for widespread information dissemination. Moreover, addressing emotional and cultural barriers through counseling and community engagement can foster a supportive environment for proactive health behaviors. Future efforts must prioritize sustained educational campaigns, longitudinal research, and the integration of advanced technologies to modernize healthcare systems and ensure equitable access to breast cancer screening and care. Through these measures, the Gulf and Middle Eastern countries can make significant strides toward reducing the burden of breast cancer and improving survival rates among women in the region.
Acknowledgments
Statement of Transparency and Principals
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Insights Into Breast Cancer in the East vs the West: A Review Yap Y, Lu Y, Tamura K, Lee JE , Ko EY , Park YH , Cao A, et al . JAMA oncology.2019;5(10). CrossRef
- Challenges with the management of young women’s breast cancer in Gulf countries and the Middle East Al Ajmi AA , Ayaad O, Al Aghbari S, Al Balushi MN , Koziha EK , Al-Ishaq Z, et al . J Young Womens Breast Cancer Health.2024;1(1&2):36-41.
- Worldwide review with meta-analysis of women's awareness about breast cancer Wang Y, Wang F, Yu L, Xiang Y, Zhou F, Huang S, Zheng C, et al . Patient Education and Counseling.2022;105(7). CrossRef
- The impact of breast cancer awareness interventions on breast screening uptake among women in the United Kingdom: A systematic review Anastasi N, Lusher J. Journal of Health Psychology.2019;24(1). CrossRef
- Breast Cancer in the Middle East: Awareness, Risk Factors, Incidence, Quality of Life, and Survival. Sobraj Publishing Service AlAjmi A, Ayaad O, Al-Baimani K. 2025. CrossRef
- Effectiveness of Mass and Small Media Campaigns to Improve Cancer Awareness and Screening Rates in Asia: A Systematic Review Schliemann D, Su TT , Paramasivam D, Treanor C, Dahlui M, Loh SY , Donnelly M. Journal of Global Oncology.2019;5. CrossRef
- Systematic Review on Knowledge and Awareness of Breast Cancer and Risk Factors Among Young Women Almutairi AH , Tamrin SBBM , Wirza R, Ahmad NB . ResearchGate.2024. CrossRef
- Awareness of Breast Cancer Risk Factors, Symptoms and Breast Self-Examination Among Omani Female Teachers: A cross-sectional study Al-Ismaili Z, Al-Nasri K, Al-Yaqoobi A, Al-Shukaili A. Sultan Qaboos University Medical Journal.2020;20(2). CrossRef
- Knowledge of symptoms, time to presentation and barriers to medical help-seeking among Omani women diagnosed with breast cancer: a cross-sectional study Al-Azri M, Al-Baimani K, Al-Awaisi H, Al-Mandhari Z, Al-Khamayasi J, Al-Lawati Y, Panchatcharam SM . BMJ open.2021;11(1). CrossRef
- Effectiveness of an Educational Program on Awareness of Breast Cancer Risk Factors, Symptoms, and Barriers to Seeking Medical Help among Adolescent Omani School Students-An Interventional Study Al-Hosni K, Chan MF , Al-Azri M. Current Oncology (Toronto, Ont.).2023;30(4). CrossRef
- Awareness about breast cancer and mammogram among women attending outpatient clinics, Ain Shams University Hospitals, Egypt Manzour AF , Gamal Eldin DA . The Journal of the Egyptian Public Health Association.2019;94(1). CrossRef
- Knowledge, attitude, and practice of breast self-examination among women attending primary health care facility in Sharkia Governorate, Egypt Orabi EEE . Egypt J Hosp Med.2024;94(1).
- Women's Breast Cancer Knowledge and Health Communication in the United Arab Emirates Abu Awwad D, Hossain SZ , Mackey M, Brennan P, Adam S. Healthcare (Basel, Switzerland).2020;8(4). CrossRef
- Knowledge and Beliefs of Cancer Risk Factors and Early Cancer Symptoms in Lebanon: A Cross-sectional Survey Among Adults in the Community Hatem G, Ghanem D, Kellen E, AlZaim I, Goossens M. Cancer Control: Journal of the Moffitt Cancer Center.2021;28. CrossRef
- Awareness of Palestinian Women About Breast Cancer Risk Factors: A National Cross-Sectional Study Elshami M, Usrof FD , Alser M, Al-Slaibi I, Okshiya HM , Ghithan RJ , Shurrab NRS , et al . JCO global oncology.2022;8. CrossRef
- Got pink? The effectiveness of health awareness campaigns on breast cancer (BC) screening in Bahrain Elgammal N. New Media Mass Commun.2023;104:46-54. CrossRef
- Assessment of University Students’ Knowledge, Attitude and Practice Regarding Breast Self-Examination in Bahrain: A Call for Action Khonji LM , Rashwan ZI , Eweida RS , Narayanan G, Darwish EM , Bayoumi MM . ResearchGate.2024. CrossRef
- Breast cancer awareness among female residents of Kuwait [Doctoral dissertation]. University of Glasgow Almajed H. 2023.
- A qualitative study to determine Kuwaiti Women's knowledge of breast cancer and barriers deterring attendance at mammography screening Marzouq Muhanna A., Floyd M. J.. Radiography (London, England: 1995).2019;25(1). CrossRef
- Breast Cancer Knowledge, Attitudes and Practices amongst Women in Qatar Hamed E, Alemrayat B, Syed MA , Daher-Nashif S, Rasheed HMA , Kane T. International Journal of Environmental Research and Public Health.2022;19(7). CrossRef
- Breast Cancer Awareness Among Women in Saudi Arabia: A Systematic Review AlRajhi B, Aljadani FF , Almarwan SR , Alzahrani AA , Sindi MHM , Kano A, Alzahrani RS , Baaqeel R. Breast Cancer (Dove Medical Press).2023;15. CrossRef
- Exploration and assessment of breast cancer awareness in the Saudi population: A cross-sectional study Elmaghraby DA , Al ben Hamad AM , Alhunfoosh KM , Alturifi HR , Albahrani MA , Alshalla AA , et al . Clin Exp Obstet Gynecol.2023;50(11):245. CrossRef
- Knowledge, Attitudes, and Practices Concerning Breast Cancer and Self Examination Among Females in UAE Kharaba Z, Buabeid MA , Ramadan A, Ghemrawi R, Al-Azayzih A, Al Meslamani AZ , Alfoteih Y. Journal of Community Health.2021;46(5). CrossRef
- Knowledge of breast cancer and self-diagnostic skills amongst women in the United Arab Emirates Al Hosani AN , Al Mazrouei NE , Behl S, Meskiri A. ResearchGate.2024. CrossRef
- Awareness About Breast Cancer Among Adult Women in Jordan Al-Najar MS , Nsairat A, Nababteh B, Essam D, Tarawneh D, Alrabadi N, Alzoubi KH . ResearchGate.2025. CrossRef
- Study of North Jordanian women's knowledge of breast cancer causes and medical imaging screening advantages Oglat AA , Hasan H, Mhanna HYA , Akhdar HF . ResearchGate.2025. CrossRef
- Beliefs, fear and awareness of women about breast cancer: Effects on mammography screening practices Emami L, Ghahramanian A, Rahmani A, Mirza Aghazadeh A, Onyeka TC , Nabighadim A. Nursing Open.2021;8(2). CrossRef
- Female high school students' knowledge and attitude toward breast cancer Mohebi Z, Heidari Sarvestani M, Moradi Z, Naghizadeh MM . BMC women's health.2023;23(1). CrossRef
- Breast Cancer Awareness Among Women Patients of a Private Hospital: A Cross-Sectional Study on Risk Factors, Symptoms, and Attitudes in TurkeyÖzel Bir Hastanenin Kadın Hastaları Arasında Meme Kanseri Farkındalığı: Türkiye'de Risk Faktörleri, Semptomlar ve Tutumlar Üzerine Kesitsel Bir Çalışma Kayıkçıoğlu H . ResearchGate.2024. CrossRef
- Breast cancer awareness among women in the Syrian Coast: a cross-sectional study Abdul Rahman S, Kherbek H, Ismail S, Abdul Rahman A, Zahlout J, Abboud I, Hraib M, et al . Annals of Medicine and Surgery (2012).2023;85(6). CrossRef
- Assessing Syrian women's knowledge of breast cancer risk factors, warning signs, and barriers to preventive measures: A cross-sectional study Bohsas H, Alibrahim H, Swed S, Khan U, Al Ibrahim M, Nashwan AJ , Hodaifah S, et al . Cancer Treatment and Research Communications.2023;36. CrossRef
- Breast cancer knowledge and practice of breast self-examination among Palestinian female, West Bank: A cross-sectional study Jobran AWM , Banat MA , Awad BY , Warasna HJ , Taqatqa YR , Jawabreh , Abualrub YR , et al . Health Science Reports.2023;6(11). CrossRef
- Cultural, Religious and Socio-Ethical Misconceptions among Muslim Women towards Breast Cancer Screening: A Systematic Review Moey S, Sowtali SN , Mohamad Ismail MF , Hashi AA , Mohd Azharuddin NS , Che Mohamed N. Asian Pacific journal of cancer prevention: APJCP.2022;23(12). CrossRef
- Comprehensive evaluation of patient‐centered care at a cancer center: A qualitative descriptive study AL-Ruzzieh MA , AL-Helih YM , Ayaad O, Haroun A, Alnaimat S. Nurs Forum.2025;2025(1):5070345.
- Assessing health literacy, learning needs, and patient satisfaction in cancer care: A holistic study in the Omani context Ayaad O, Ibrahim R, AlHasni NS , Salman BM , Sawaya ZG , Al Zadjali R, et al . Asian Pac J Cancer Biol.2024;9(4):553-560. CrossRef
- Higher and Middle Management Perspectives on Patient-Centered Care in an Oncology Setting: A Qualitative Study AL-Ruzzieh MA , AL-Helih YM , Haroun A, Ayaad O. Nursing Reports.2024.
- Predicting and classifying the perceptions of learning needs importance in cancer patients; a machine learning approach Ayaad O, Ibrahim R, AlBaimani K, AlGhaithi MM , Sawaya ZG , AlHasni NS , et al . Health Educ Health Promot.2024;12(4):649-660.
- The implications of artificial intelligence in the quality of health services Ayaad O. Innov Multidiscip J Sci Technol.2024;1(1):1-9.
- Impact of nurses' emotional intelligence on the implementation of a professional practice model in cancer care Al-Ruzzieh MA , Ayaad O. British Journal of Nursing (Mark Allen Publishing).2021;30(19). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2025
Author Details