Epidemiological Analysis of Prostatic Cancer: Incidence, Prevalence, Mortality, and Disability Burden in Middle Eastern Countries
Download
Abstract
Prostatic cancer is considered the second most common cancer among men worldwide. It has significant geographical variability in its burden. Using data from the Global Burden of Disease (GBD) 2021 database, this review aimed to analyze the epidemiological burden of prostatic cancer in 14 Middle Eastern countries. The data of incidence, prevalence, mortality, and age-standardized disability-adjusted life years (DALYs) were analyzed. Compared to the global average rate of 33.449 per 100,000, our results showed that the Middle East reports a lower average incidence rate of 17.297 per 100,000 population. However, outliers such as Lebanon (64.381 per 100,000) and Turkey (52.166 per 100,000) exhibit a significantly higher burden. Mortality and age-standardized DALYs also highlight disparities, with Lebanon and Turkey recorded a higher values compared to other regional counterparts. Conversely, countries like Oman and Yemen reported the lowest rates, potentially reflecting underdiagnosis or limited healthcare access. The results underscore the importance of enhancing early detection programs, such as prostate-specific antigen (PSA) testing, and addressing modifiable risk factors, including smoking and obesity. By bridging gaps in data and healthcare access, this research highlights critical areas for policy interventions and targeted public health strategies to reduce the burden of prostatic cancer in the region. The findings provide valuable insights to inform regional healthcare planning and resource allocation, contributing to a broader understanding of global prostatic cancer epidemiology.
Introduction
Prostatic cancer represents a significant global health concern, ranking as one of the most prevalent cancers among men worldwide. In 2020, it was estimated that 1.4 million new cases of prostatic cancer were diagnosed globally, making it the second most frequently diagnosed cancer in men and the fifth leading cause of cancer-related deaths [1]. In the Middle East, more than 50000 newly diagnosed cases with prostatic cancer were reported in 2020, representing a 3.7% of the global incidence rates [2]. The disease’s incidence, prevalence, and mortality exhibit substantial geographical variability, influenced by factors such as genetic predisposition, environmental exposures, lifestyle, and healthcare access. Genetic predispositions, particularly BRCA1 and BRCA2 mutations, have been identified as potential risk factors for aggressive forms of prostatic cancer. Studies suggest that these mutations are more prevalent in certain Arab populations, contributing to variations in disease incidence and severity. In particular, the Middle East region presents unique challenges and disparities in the epidemiological burden of prostatic cancer that warrant focused investigation [2-4].
The global burden of prostatic cancer has been on the rise, driven by aging populations, increased life expectancy, and improved diagnostic capabilities [5, 6]. However, in the Middle East and North Africa (MENA) region, the reported burden appears lower than the global average. This disparity raises questions about the adequacy of cancer detection, reporting practices, and potential underdiagnosis [3, 7]. Understanding the true burden in this region is critical for effective policy formulation and resource allocation.
Despite the lower reported incidence and prevalence rates in many Middle Eastern countries compared to global figures, certain nations like Lebanon and Turkey have notably higher rates, surpassing global averages [4, 8]. These variations suggest the influence of diverse healthcare systems, environmental factors, and sociocultural determinants across the region. However, the literature lacks comprehensive studies that systematically examine these disparities and their underlying causes [5, 9].
The Middle East’s demographic and epidemiological transitions are creating new health challenges, including an increasing cancer burden. Prostatic cancer is particularly relevant in this context, as its risk factors, such as aging, obesity, and dietary habits, are becoming more prevalent in the region [6, 7]. The limited availability of region-specific data has hindered the development of targeted public health strategies, emphasizing the need for robust epidemiological research.
This study addresses the significant gap in the literature by analyzing the epidemiological burden of prostatic cancer in the Middle East using data from the Global Burden of Disease (GBD) 2021 database. By focusing on metrics such as incidence, prevalence, mortality, and disability-adjusted life years (DALYs), this research provides a comprehensive overview of the disease’s impact across 14 countries in the region. This analysis is pivotal in identifying priority areas for intervention and policy-making [3, 10].
Prostatic cancer carries substantial societal and economic implications, given its chronic nature and potential to cause significant morbidity and mortality. In regions like the Middle East, where healthcare resources may be limited, understanding the disease’s burden can guide investments in screening programs, healthcare infrastructure, and patient education [5, 11]. Furthermore, disparities in healthcare access across countries highlight the importance of equitable health initiatives tailored to local needs.
The findings of this study hold significant implications for public health planning. By quantifying the burden of prostatic cancer in the Middle East, this research underscores the need for improved cancer registries, early detection programs, and access to treatment. Additionally, it highlights the importance of addressing lifestyle risk factors such as smoking and obesity, which are becoming increasingly prevalent in the region [3, 12].
This research also aims to contribute to the global understanding of prostatic cancer epidemiology by providing region-specific insights that can inform international comparisons. Understanding regional variations in disease burden is essential for tailoring prevention and treatment strategies and for fostering collaboration among countries with shared health challenges [4, 13].
The purpose of this study is to bridge the knowledge gap regarding the epidemiological characteristics of prostatic cancer in the Middle East, thereby supporting evidence-based policymaking and resource allocation. By leveraging robust data from the GBD 2021 database, this study not only enhances our understanding of the current burden but also identifies key areas for future research and intervention [3, 5, 14, 15].
Methods
We analyzed data from the Global Burden of Disease (GBD) database compiled by the Institute of Health Metrics and Evaluation at the University of Washington, Seattle (www.healthdata.org). We utilized the GBD 2021 data to extract the incidence, prevalence mortality, and disability-adjusted life years (DALYs) of prostatic cancer in Middle Eastern countries for the year 2021 and presented it through a set of meaningful descriptive statistics. Though the GBD data are one of the most rigorous and comprehensive data sets in the world, data limitations in terms of validity and reliability could arise especially in conflict zones of the world like Yemen, and Iraq.
Our analysis focused on the following countries in the Middle East: Bahrain, Egypt, Iran (Islamic Republic of Iran) Iraq, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, Syrian Arab Republic, Turkey, United Arab Emirates, and Yemen. Data were initially downloaded into Microsoft Excel and subsequently analyzed using SPSS statistical software (IBM SPSS, Inc., Chicago, 2021). While GBD data are among the most comprehensive and rigorous datasets available, limitations exist, particularly in conflict-affected regions such as Yemen, Syria, and Iraq. Data collection challenges in these areas, including underreporting, healthcare infrastructure constraints, and political instability, may introduce estimation biases and understate the actual burden of prostatic cancer.
By leveraging the comprehensive data from the GBD 2021, this study provides valuable insights into the current state of prostatic cancer in the Middle East, identifies key areas of concern, and underscores the need for targeted public health interventions to address the growing health challenges among males in the region. We applied descriptive statistics, including mean, standard deviation, and interquartile range, to summarize the data. Additionally, regression models were used to assess associations between prostatic cancer burden and key risk factors such as healthcare access, obesity prevalence, and smoking rates.
Results
Incidence
Table 1 shows that the incidence rates per 100,000 population reveal notable variations across countries in the Middle East region, with the global average serving as a baseline for comparison. Globally, the incidence rate is 33.449 per 100,000 population, while the regional average for the Middle East is 20.626 per 100,000 population, indicating a generally lower burden of new cases in this region.
| location | Incidence | Prevalence | Mortality | DALYs (Disability-Adjusted Life Years) |
| Bahrain | 25.134 | 209.4 | 4.205 | 103.185 |
| Egypt | 9.225 | 67.847 | 3.202 | 67.848 |
| Iran (Islamic Republic of) | 24.777 | 192.124 | 7.97 | 149.302 |
| Iraq | 8.64 | 64.564 | 2.523 | 52.995 |
| Jordan | 12.857 | 105.378 | 2.953 | 62.739 |
| Kuwait | 25.436 | 215.527 | 4.487 | 89.791 |
| Lebanon | 64.381 | 480.64 | 20.494 | 332.828 |
| Oman | 4.676 | 38.341 | 0.834 | 20.16 |
| Palestine | 17.422 | 132.53 | 5.092 | 106.257 |
| Qatar | 16.353 | 143.68 | 1.877 | 50.865 |
| Saudi Arabia | 8.259 | 69.399 | 1.182 | 30.117 |
| Syrian Arab Republic | 25.939 | 206.577 | 7.084 | 145.805 |
| Turkey | 52.166 | 410.955 | 13.75 | 265.365 |
| United Arab Emirates | 9.439 | 81.947 | 1.723 | 50.348 |
| Yemen | 4.694 | 30.406 | 2.57 | 51.469 |
| The Middle East | 20.626 | 163.288 | 5.32973 | 105.272 |
| Global | 33.449 | 262.351 | 10.922 | 205.627 |
Source, Global burden of disease study 2021 results. Retrieved from https://www.healthdata.org
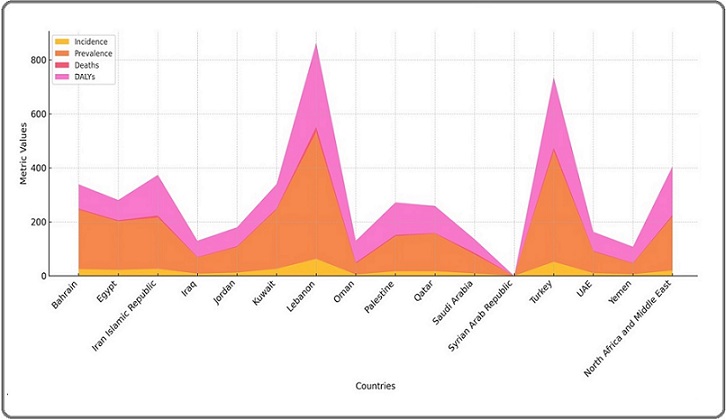
Within the region, Lebanon stands out with the highest incidence rate of 64.381 per 100,000 population, nearly double the global average. This suggests specific health challenges, potentially driven by environmental, socioeconomic, or healthcare factors. Similarly, Turkey, with an incidence rate of 52.166 per 100,000 population, also exceeds the global average, highlighting a significant burden of new cases (Figure 1 and Figure 2).
Figure 1. Comparative Health Metrics by Country: Prostatic Cancer Incidence, Prevalence, Deaths, and Disability Burden (DALYs) in Middle Eastern countries.
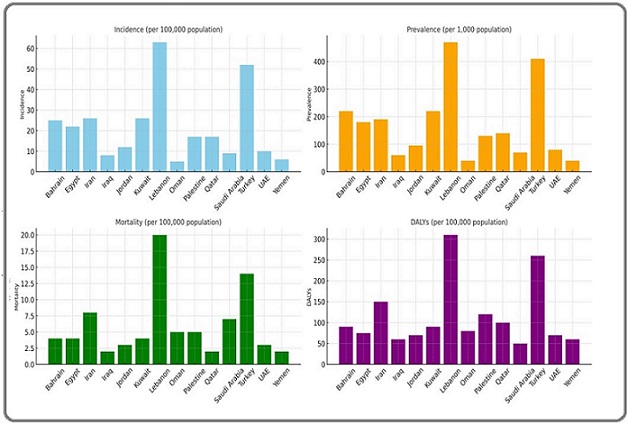
Figure 2. Comparative Health Metrics by Country by Stacked Area Chart.
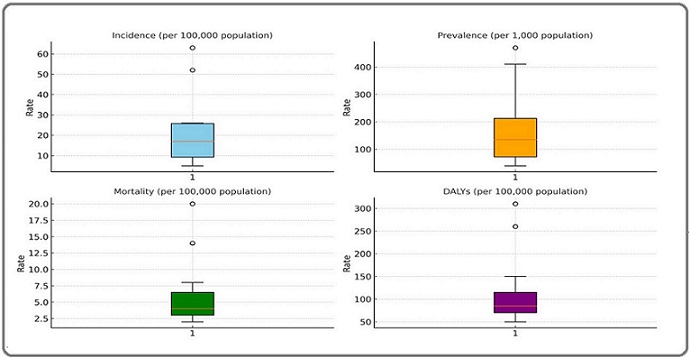
Both countries are considered as outliers (Figure 3).
Figure 3. Distribution of Prostatic Cancer Middle in Middle East. Incidence Rates: - High Outliers: Lebanon (64.38), Turkey (52.17). - Median Range: Jordan (12.86), Palestine (17.42), Qatar (16.35). - Lower Quartile Range: Egypt (9.22), UAE (9.44), Saudi Arabia (8.26). - Lowest Rates: Oman (4.68), Yemen (4.69). Mortality: - High Outliers: Lebanon (20.49), Turkey (13.75). - Median Range: Kuwait (4.49), Bahrain (4.20), Palestine (5.09). - Lower Quartile Range: Egypt (3.20), Saudi Arabia (1.18), UAE (1.72). - Lowest Rates: Oman (0.83), Yemen (2.57). DALYs (Disability-Adjusted Life Years): - High Outliers: Lebanon (332.83), Turkey (265.37). - Median Range: Iran (149.30), Syria (145.80), Palestine (106.26). - Lower Quartile Range: Egypt (67.85), Saudi Arabia (30.12), Qatar (50.87).- Lowest Values: Oman (20.16), Yemen (51.47). Prevalence Rates: - High Outlier: Lebanon (480.64). - Median Range: Kuwait (215.53), Bahrain (209.40), Iran (192.12), Syria (206.58). - Lower Quartile Range: Egypt (67.85),UAE (81.95), Saudi Arabia (69.40), Jordan (105.38). - Lowest Rates: Oman (38.34), Yemen (30.41)..
Other countries such as Bahrain (25.134), Iran (24.777), Syrian Arab Republic (25.939), and Kuwait (25.436) report moderate incidence rates, slightly below the global average but higher than the regional average. These rates suggest a consistent burden of new cases across these nations. In contrast, countries like Oman (4.676), Yemen (4.694), and Egypt (9.225) report the lowest incidence rates, significantly below both the regional and global averages.
Lebanon and Turkey stand out as high outliers with incidence rates of 64.38 and 52.17, respectively, indicating a significant disease burden compared to other countries. In contrast, countries like Jordan (12.86), Palestine (17.42), and Qatar (16.35) exhibit incidence rates closer to the median, reflecting moderate levels of disease occurrence. Meanwhile, Egypt (9.22), UAE (9.44), and Saudi Arabia (8.26) fall within the lower quartile range, showcasing comparatively lower rates. The lowest incidence rates are observed in Oman (4.68) and Yemen (4.69), which are near the lower whisker, suggesting minimal disease occurrence.
Prevalence
The prevalence rate per 1,000 population highlights significant variability across countries in the Middle East countries (Figure 1-4) [5, 6-9].
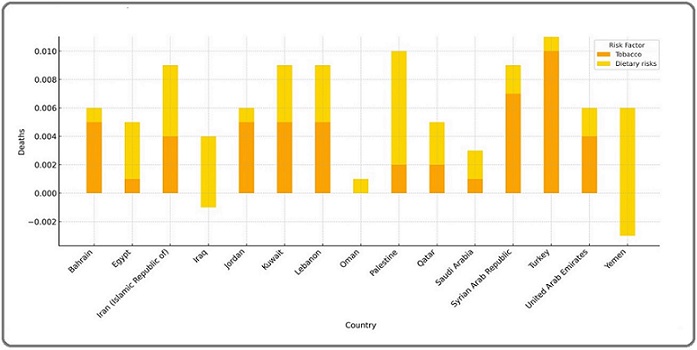
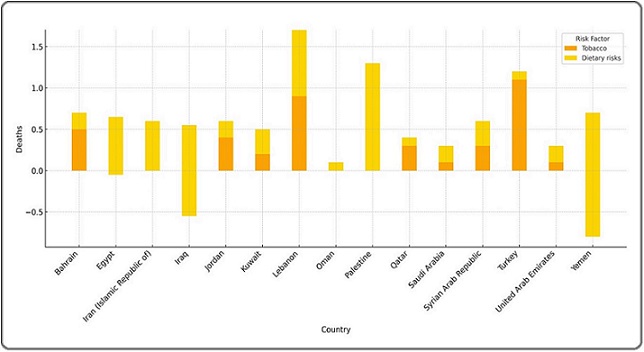
Figure 4. Impact of Dietary Risks and Tobacco on Mortality Across Countries in the 15-49 Years Group.
While the global average prevalence is 262.351 per 1,000 population, the regional average is notably lower at 163.288 per 1,000 population, indicating a generally reduced burden of ongoing health conditions. However, certain countries in the region, such as Lebanon (480.640) and Turkey (410.955), report prevalence rates well above the global and regional averages, reflecting a substantial proportion of their populations affected by chronic or ongoing illnesses. Countries like Kuwait (215.527), Bahrain (209.400), and the Syrian Arab Republic (206.577) also have a higher prevalence rates, suggesting a considerable health burden likely linked to lifestyle factors, healthcare access, and disease detection practices.
In contrast, countries such as Oman (38.341) and Yemen (30.406) reported the lowest prevalence rates, significantly below the global and regional averages. These figures could indicate a genuinely lower disease burden or underreporting due to limited healthcare access or diagnostics. Moderate prevalence rates are observed in countries like Qatar (143.680) and Palestine (132.530), which align closely with the regional average.
Mortality
The number of deaths per 100,000 population varies significantly across countries in the Middle East region, with the regional average at 5.32973 deaths, considerably half the global average rate of 10.922 deaths. Countries like Lebanon (20.494) and Turkey (13.750) reported the highest mortality rates in the region, significantly exceeding both the regional and global averages. This could reflect a higher burden of chronic illnesses, ongoing conflicts, or environmental factors contributing to mortality. Similarly, Iran (7.970) and the Syrian Arab Republic (7.084) also report higher death rates compared to the regional average, likely driven by health system challenges or long-term impacts of war and political instability.
Conversely, countries like Oman (0.834), Qatar (1.877), and the United Arab Emirates (1.723) report some of the lowest mortality rates in the region, reflecting better healthcare systems, fewer conflicts, and higher standards of living. Moderate mortality rates are observed in Bahrain (4.205), Kuwait (4.487), and Palestine (5.092), aligning more closely with the regional average.
Disability-Adjusted Life Years (DALYs)
The Disability-Adjusted Life Years (DALYs) and Years Lived with Disability (YLDs) reveal significant health disparities across countries in the Middle East region. The regional average for DALYs is 105.272 per 100,000 population, much lower than the global average of 205.627, indicating a comparatively lower overall health burden. However, countries like Lebanon (332.828) and Turkey (265.365) reported DALYs far exceeding both the regional and global averages, reflecting high burdens of disease and premature mortality. Similarly, Iran (149.302) and the Syrian Arab Republic (145.805) also have elevated DALYs, likely driven by chronic health conditions, conflict, and systemic healthcare challenges. In contrast, countries like Oman (20.160), Saudi Arabia (30.117), and the United Arab Emirates (50.348) report the lowest DALYs, highlighting stronger healthcare systems and reduced disease burdens.
Impact Dietary Risks and Tobacco on Mortality Across Age Groups and Countries
The comparison of deaths due to Dietary Risks and Tobacco across countries highlights significant differences in their impact on mortality in the (15-49) and (50-74) age groups. In the (15-49) years group, Tobacco consistently shows a positive effect on deaths, with countries like Turkey (0.011) and the Syrian Arab Republic (0.009) experiencing higher tobacco-related mortality rates. On the other hand, Dietary Risks often show negative values, such as in Yemen (-0.0098) and Palestine (-0.0087), indicating either minimal or protective effects in this younger age group. These trends suggest that younger populations may experience fewer dietary-related deaths and more significant risks from tobacco consumption (Figure 4).
In the (50-74) years group, the impact of both risk factors becomes more pronounced. Tobacco contributes significantly to mortality, with high rates in Lebanon (1.768) and Turkey (1.159), reflecting the cumulative effects of long-term smoking. Conversely, Dietary Risks also show stronger protective trends in older populations, with countries like Yemen (-1.616) and Palestine (-1.375) reporting negative values. However, in countries like Egypt (-0.675) and Iran (-0.289), the reduction in deaths due to dietary factors is less pronounced. These findings emphasize the need for age-specific health interventions, with a focus on smoking cessation in older populations and preventive dietary measures across all age groups (Figure 5).
Figure 5. Impact of Dietary Risks and Tobacco on Mortality Across Countries in the 50-74 Years Group.
Discussion
The analysis of prostatic cancer in the Middle East countries highlighted several critical findings regarding the incidence, prevalence, mortality, and DALYs, showcasing distinct patterns and disparities within the region. Lebanon and Turkey emerged as high-burden countries, indicating specific challenges in managing this disease. These elevated rates may reflect a combination of lifestyle factors, environmental exposures, and healthcare access disparities. In contrast, countries like Oman and Yemen reported notably lower metrics, potentially indicating underdiagnosis or systemic healthcare limitations [8, 9]. When compared to high-income countries, the Middle East shows both unique strengths and weaknesses. While some countries demonstrate low mortality and DALYs, likely due to efficient healthcare systems, others reflect significant gaps in detection and management. For example, high-income nations have long employed PSA screening programs, resulting in early detection and lower mortality rates. However, such screening remains less widespread in the Middle East, affecting overall outcomes [5, 11, 16]. Though, the adoption of PSA screening program could affect the proper utilization of such test method and ends up with false positive and over treatment cases, we recommend judicious adoption of such methodologies and countries can conduct specific risk-benefit analysis to adopt the most proper methodology [2, 3].
While prostate-specific antigen (PSA) screening is a valuable tool for early detection of prostatic cancer, it also carries significant risks of overdiagnosis and overtreatment. PSA levels can be elevated due to benign conditions such as benign prostatic hyperplasia (BPH) and prostatitis, leading to false positives that may result in unnecessary anxiety, additional testing, and invasive procedures [3, 4].
Overdiagnosis occurs when low-risk, indolent cancers which may never progress to cause harm are detected and treated unnecessarily. This can lead to overtreatment, including surgery, radiation therapy, and hormone therapy, all of which carry risks such as urinary incontinence, erectile dysfunction, and other complications that impact patients’ quality of life [4, 5].
To mitigate these risks, PSA screening should be carefully targeted, focusing on high-risk populations (e.g., those with a family history or BRCA mutations) and incorporating risk stratification tools such as multiparametric MRI and genomic testing. Shared decision-making between patients and healthcare providers is essential to weigh the benefits and risks of PSA screening, ensuring that only clinically significant cancers are treated while avoiding unnecessary interventions for low-risk cases [3-5].
The elevated prevalence rates in Lebanon and Turkey may point to prolonged survivorship in these countries, suggesting advancements in managing chronic cancer conditions. However, the high burden also indicates the need for improved early detection systems and comprehensive treatment options. Comparatively, countries like the United States demonstrate higher prevalence but lower mortality, underscoring the effectiveness of early intervention [14, 17].
Mortality trends in the Middle East highlight critical disparities. Lebanon’s and Turkey’s mortality rates exceed the global average, reflecting possible late-stage diagnoses and inadequate access to state-of-the-art treatments [17-20]. This trend contrasts with countries like the UAE and Oman, which maintain some of the lowest mortality rates in the region. This disparity underscores the need for equitable healthcare distribution and resource allocation within the Middle East [3, 10].
DALYs, as a measure of both fatal and nonfatal outcomes, provide deeper insights into the burden of prostatic cancer. Lebanon and Turkey report alarmingly high DALYs, indicative of severe disease impacts on quality of life and productivity [20-22]. In contrast, lower DALYs in the Gulf Cooperation Council (GCC) countries like the UAE and Saudi Arabia may reflect stronger healthcare systems and preventive measures. These findings align with global patterns where nations with higher healthcare investments report reduced DALYs [1, 8].
Tobacco use was identified as a significant risk factor, particularly in Turkey and Syria. The association between long-term smoking and cancer incidence is well-documented globally, emphasizing the importance of robust tobacco control policies. In contrast, dietary factors showed mixed effects across age groups, reflecting the cultural and nutritional diversity within the region. Addressing these modifiable risks could significantly reduce prostatic cancer burden [15, 23].
Lebanon and Turkey report significantly higher incidence, mortality, and disability-adjusted life years (DALYs) for prostatic cancer compared to other Middle Eastern countries, diverging from regional trends due to multiple factors. Both countries have high levels of urbanization, leading to increased exposure to environmental pollutants, sedentary lifestyles, and reduced physical activity, all of which are established risk factors for prostatic cancer. Additionally, Westernized dietary patterns, including high-fat diets, processed foods, and increased red meat consumption, have become more prevalent in Lebanon and Turkey, contributing to metabolic changes and hormonal imbalances associated with increased cancer risk. Moreover, higher screening rates and better healthcare access in these countries may lead to more early diagnoses, thereby increasing reported incidence rates. In contrast, underdiagnosis in other Middle Eastern countries with limited screening programs may mask the true burden of the disease. These combined factors highlight the need for tailored public health interventions that address lifestyle risk factors while ensuring equitable access to screening and early detection programs across the region [3-5].
Healthcare access emerged as a consistent determinant of outcomes. Countries with well-established healthcare systems, such as the UAE and Qatar, report lower incidence and mortality, mirroring trends in high-income countries. Conversely, conflict-affected nations like Yemen and Syria face significant challenges, including underreporting and limited healthcare infrastructure. These issues highlight the intersection of health and geopolitics in shaping cancer outcomes [3, 13].
The findings underscore the critical need for region- specific strategies, including the establishment of cancer registries to improve data accuracy. Accurate epidemiological data are essential for tracking disease trends and designing effective interventions. In high- income nations, such registries have facilitated targeted public health measures, a model that could be adapted to the Middle East [10, 14].
Public health policies targeting prostatic cancer should prioritize early detection and prevention. Lessons from developed countries reveal the effectiveness of PSA screening programs, coupled with public awareness campaigns, in reducing advanced-stage diagnoses. While such programs are resource-intensive, their long-term benefits in reducing disease burden are well-documented [5, 11, 24, 25].
Lastly, addressing lifestyle risk factors such as smoking, obesity, and sedentary habits is crucial. These factors are becoming increasingly prevalent in the Middle East, driven by urbanization and changing lifestyles [25-28]. This may explain the high rate of prostatic cancer in Lebanon and Turkey. In a national study to assess the dietary habits of the Lebanese population, the authors reported the widespread of unhealthy dietary life styles that include high sugar, unsaturated fats, processed meats and poor in vitamins [17, 26]. A comparable unhealthy dietary habit was reported among students attending the health colleges in which more than half of the study participants were routinely consuming fast foods (12, 18). Public health initiatives focusing on education, lifestyle modifications, and tobacco cessation could substantially reduce the future burden of prostatic cancer in the region [29, 30].
In conclusion, this study highlights the significant variability in the epidemiological burden of prostatic cancer across the Middle East, with pronounced disparities between countries. Lebanon and Turkey stand out as high-burden nations, emphasizing the need for enhanced healthcare infrastructure, early detection programs, and targeted interventions. In contrast, the low burden reported in countries like Oman and Yemen may reflect systemic challenges such as underreporting or limited diagnostic capabilities. These findings underscore the need for region-specific strategies to address healthcare disparities and improve cancer outcomes. An example of a cost-effective strategy is the adoption of telemedicine, which can enhance access to healthcare for individuals in rural and underserved areas, ensuring timely consultations and follow-ups. Additionally, subsidized PSA testing programs, particularly for high-risk populations, can improve early detection without imposing significant financial burdens on patients or healthcare systems.
By comparing Middle Eastern countries to global trends, this study reveals critical gaps in cancer prevention and management within the region. Efforts to reduce the prostatic cancer burden must prioritize early detection, equitable healthcare access, and public health campaigns targeting modifiable risk factors. Cultural adaptation of public health campaigns is essential to overcome social stigma associated with cancer screening and encourage participation in preventive healthcare. This includes community engagement, religious leader involvement, and awareness programs tailored to local beliefs and values to increase screening uptake and lifestyle modifications. Investments in robust cancer registries and surveillance systems will be crucial to accurately monitor disease trends and guide evidence-based policies. Ultimately, addressing these challenges through cost-effective, accessible, and culturally sensitive interventions will not only benefit the Middle East but also contribute to the global effort to reduce the burden of prostatic cancer.
Acknowledgments
Statement of Transparency and Principals
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Estimating the global cancer incidence and mortality in 2020: GLOBOCAN sources and methods Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM , Piñeros M, et al . Int J Cancer.2020;149(3):778-89. CrossRef
- Burden of prostate cancer in the Middle East: A comparative analysis based on global cancer observatory data Kearney G, Chen M, Mula-Hussain L, Skelton M, Eren MF , Orio PF , Nguyen PL , D'Amico AV , Sayan M. Cancer Medicine.2023;12(23). CrossRef
- Comprehensive review of cardiovascular disease in prostate cancer: epidemiology, risk factors, therapeutics and prevention strategies Moryousef J, Duivenvoorden W, Leong D, Pinthus JH . Prostate Cancer and Prostatic Diseases.2024. CrossRef
- Descriptive epidemiology of prostate cancer in India, 2012-2019: Insights from the National Cancer Registry Programme Sankarapillai J, Krishnan S, Ramamoorthy T, Sudarshan KL , Mathur P. Indian journal of urology: IJU: journal of the Urological Society of India.2024;40(3). CrossRef
- Prostate cancer across four countries in the Middle East: a multi-centre, observational, retrospective and prognostic study El-Karak F, Shamseddine A, Omar A, Haddad I, Abdelgawad M, Naqqash MA , Kaddour MA , Sharaf M, Abdo E. Ecancermedicalscience.2024;18. CrossRef
- The burden of prostate cancer in the North Africa and Middle East Region from 1990 to 2021 Safiri S, Shamekh A, Hassanzadeh K, Fazlollahi A, Sullman MJM , Raeisi M, Kolahi A. Scientific Reports.2025;15(1). CrossRef
- Awareness of prostate cancer and its screening tests in men in the Middle East: A systematic review and meta-analysis Mohamed NSA , Asfari JNO , Sambawa SMA , Aljurf RMD , Alsaygh KAA , Arafah AM . Journal of Family & Community Medicine.2025;32(1). CrossRef
- Disparities in cancer epidemiology and control in the Middle East and North Africa region: A systematic review Al-Rifai R, Abulaban A, Nasrallah A. BMC Cancer.2021;21(1):554. CrossRef
- The survey of effect of combination therapy with tamsulosin – finasteride compared with tamsulosin alone on symptom improvement of benign prostatic hypostatic Sabbagh AJ , Khalighinezhad M. Immunopathologia Persa.2018;4(2). CrossRef
- Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries Bray F, Ferlay J, Soerjomataram I, Siegel RL , Torre LA , Jemal A. CA: a cancer journal for clinicians.2018;68(6). CrossRef
- A case report to a successful surgical treatment of non-catheter dependent benign prostatic hyperplasia as a cause of non-dilated obstructive uropathy Fijasri NH , Daud MAM , Zain WZW , Merican SRHI , Mohamad IS . Journal of Renal Injury Prevention.2021;11(4). CrossRef
- Effects of combined ethanol extract of Funtumia africana and Abutilon mauritianum leaves on prostate biomarkers and serum mineral levels in prostatic hyperplasia induced male rats Uroko RI , Adamude FA , Egba SI , Nwuke CP , Asadu CL , Anyaorah P. Journal of Renal Endocrinology.2020;7(1). CrossRef
- GBD 2021 data, Institute of Health Metrics and Evaluation. Global burden of disease study 2021 results ;:2021. Available from: https://www.healthdata.org.
- Epidemiology and burden of cancer in the MENA region Abdel-Rahman O, Mahmoud O, Karim S. J Glob Oncol.2022;8(1):123-30. CrossRef
- Cancer detection challenges in the Middle East: Lessons from regional studies Mousavi SM , Mohagheghi MA , Pourhosseini SJ . Public Health Rev.2021;42:1-13. CrossRef
- Cancer statistics and trends worldwide: Implications for public health interventions Jemal A, Miller KD , Siegel RL . Lancet Oncol.2020;21(2):230-40. CrossRef
- Trends in cancer incidence in the Middle East: Implications for public health interventions Al-Madouj A, Al-Zahrani A, Al-Hamdan N. Cancer Epidemiol.2019;60:56-64. CrossRef
- Health transitions and cancer prevalence in the Middle East: A demographic perspective Omran AR , Al-Hassan S, Musa T. Glob Health J.2020;14(3):45-58. CrossRef
- Bridging the cancer care gap: Insights from Middle Eastern studies Smith BD , Habib MS , El-Ghannam A. World J Clin Oncol. 2022;13(5):412–28.2022;13(5):412-28. CrossRef
- Risk factors for prostate cancer in Middle Eastern populations: A meta-analysis Hassen T, Ibrahim H, Youssef Z. Asian Pac J Cancer Prev.2021;22(4):1101-1109. CrossRef
- Evaluation of the urine mRNA-PCA3 expression level in prostate patients; comparison between benign prostatic hyperplasia and cancer Yazdani A, Namdari F, Gorgani-Firuzjaee S, Niroomand H. Immunopathologia Persa.2022;8(2). CrossRef
- Flexible cystodiathermy for the treatment of recurrent superficial bladder transitional cell carcinoma; efficacy, safety, and cost-effectiveness Ayyad M, Ayaad O, Alkhatatbeh H, Qaddumi B, Sawaqed F, Al-Rawashdeh S. Journal of Renal Injury Prevention.2025;14(4). CrossRef
- The effectiveness of gabapentin in treating overactive bladder: a quasi-experimental study Ayyad M, Ayaad O, Alkhatatbeh H, Sawaqed F, Al-Rawashdeh S, Qaddumi B. Immunopathologia Persa.2023;10(1). CrossRef
- Dietary Intake among Lebanese Adults: Findings from the Updated LEBANese natiONal Food Consumption Survey (LEBANON-FCS) Hoteit M, Khattar M, Malli D, Antar E, Al Hassani Z, Abdallah M, Hachem D, et al . Nutrients.2024;16(11). CrossRef
- Laparoscopic Partial Nephrectomy: Off-Clamp Versus on Clamp Ayyad M, Ayaad O, Alkhatatbeh H, Sawaqed F, Al-Rawashdeh S. Asian Pacific journal of cancer prevention: APJCP.2022;23(5). CrossRef
- Association between serum vitamin D levels and prostate tumor: a systematic review and meta-analysis Ghaderi R, Abdollahi Z, Madani MH , Doshantapeh AG , Moghimi B, Jarang M, Rezaei J, Ghaffariyan S, Arismani RJ . Journal of Renal Injury Prevention.2024;13(3). CrossRef
- The association between systemic immune-inflammation index and risk of prostate carcinoma; a systematic review and meta-analysis Nourmohammadi A, Azimi SA , Kareem RA , Badraldeen SQ , Arismani RJ , Roohinezhad R, Pourmasomi H, Attar A, Vahdati SS . Immunopathologia Persa.2025;11(2). CrossRef
- Measuring quality of life among patients with urinary stone disease; A qualitative study Ayyad M, Ayaad O. Journal of Renal Injury Prevention.2022;12(4). CrossRef
- Assessing Health Literacy, Learning Needs, and Patient Satisfaction in Cancer Care: A Holistic Study in the Omani Context Ayaad O, Ibrahim R, AlHasni NS , Salman BM , Sawaya ZG , Al Zadjali R, et al . ResearchGate.2025. CrossRef
- Predicting and Classifying the Perceptions of Learning Needs Importance in Cancer Patients; a Machine Learning Approach Ayaad O., Ibrahim R., AlBaimani Kh, AlGhaithi M. M., Sawaya Z. G., AlHasni N. S., AlAwaisi H. S., et al . Health Education and Health Promotion.2024;12(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2025
Author Details