Surface Mould Brachytherapy in Superficial Tumors, Case Series from a Tertiary Cancer Centre in North India with Review of Literature
Download
Abstract
Purpose: To evaluate the efficacy of surface mould brachytherapy (SMB) in the management of superficial tumors, particularly in anatomically challenging locations, in the era of advanced radiotherapy technologies.
Methods: Present study is a retrospective review of case series of ten patients with early stage and recurrent diseases of various sites that were treated with surface mould brachytherapy. Three patients of different disease sites were selected for reporting. All patients underwent individualized CT-based planning. All of them were treated using Ir-192 high dose rate (HDR) SMB at our center.
Results: We followed up the patients at 1st, 3rd, 6thmonth and then yearly thereafter. Among all the ten cases there were two local recurrences, three cases died of metastatic disease and five were disease free till last follow up at two years. Skin reactions of grade 2 and 3 were reported during treatment which subsided after 2 to 3 weeks of treatment.
Conclusion: SMB is a very effective treatment for early-stage disease and treating carcinoma of skin where difficult curve surfaces are involved. It is effective in treatment of solitary recurrences of disease and also helpful in organ preservation.
Introduction
As per GLOBOCAN cancer statistics 2022 skin malignancy (non melanoma skin cancers excluding basal cell carcinoma) is on the rise in the world with incidence of 744792 males and 489803 females [1]. Superficial tumors involving skin have low metastatic potential, but can spread locally resulting in significant morbidity and disfigurement. Surgery has excellent local control (LC) rates - generally 95% and less overall treatment time. Mohs microsurgery has excellent control rates to the tune of 95-99% but has higher failure rates for tumors that are multicentric, disconnected foci, or give rise to metastases or satellite lesions [2]. Multiple other options are available for treating skin malignancies, among which both external beam radiotherapy (EBRT) techniques as well as brachytherapy (BT) is the lesser explored option [3].
However, there are scenarios where surgery is not feasible, due to cosmetic outcome or functional status postsurgery (ex. tumors on the ears, nose, eyelids) or patient factors (elderly patients, or those with comorbidities) [3-7]. In recent years, technological advances have improved the ability to deliver safe and effective radiotherapy, resulting in renewed interest in this modality [3, 4, 8-9]. BT techniques deposit a significantly higher dose within a tumor, with better sparing of adjacent normal structures versus plans using external beam radiotherapy (EBRT) or electron therapy. BT has the advantage of sharp dose fall off and is indicated forlesions located at, or just below the skin surface. Lesions upto 5mm are well treated by mould radiotherapy whereas lesions greater than 5 mm require interstitial techniques [10-11]. BT is also a good alternative for preservation of functional structures not possible with surgery [12]. HDR brachytherapy delivers a highly conformal plan with higher biologically equivalent doses and has also shown high local control (LC) rates (83-100%) [13-15].
BT in the treatment of superficial skin tumors is an excellent modality for cosmetically challenging sites and locally recurrent tumors but randomized controlled trials, systematic reviews and/or metanalyses are lacking in literature. The aim of this review is to present case series of ten cases with detailed description of three different types of cases treated using 192Ir-based HDR SMB at our institution with systematic review of literature.
Materials and Methods
We selected ten cases of histologically proven cases of superficially limited carcinoma taken for SMB from Jan 2019 to Dec 2021 (Table 1).
| Cases | Type of cancer | Number |
| Skin malignancies | Squamous and basal cell carcinoma | 5 |
| Recurrent cancer | Local skin recurrence (breast and penile cancer) | 3 |
| Primary Penile cancer | Squamous cell carcinoma | 2 |
Three out of ten cases were selected for detailed description on the basis of site and type of malignancy. Metastatic workup was done for all the patients. All patients were subjected for planning CT scan to confirm the depth of tumor invasion not more than 5 mm. Thermoplastic cast in part or whole was used to conform to the shape and assure reproducibility. The surface area of the tumor to be treated was marked by a copper wire. Remodelling wax was used to take care of any air gaps over the intended treatment area and fixing the flexible catheters. Flexible catheters (2mm diameter) were placed at one cm and fixed to the underlying layer of thermoplastic cast with modelling wax.
CT simulation was done taking 1 mm cuts and images were transferred to Oncentra brachytherapy planning system.
Contouring of the gross target volume (GTV) was done based on the radio opaque wire and radiology findings. A 5 mm margin was given around GTV to generate clinical target volume (CTV). No expansion to CTV was given to generate Planning Target volume (PTV). Surrounding organ at risk was also contoured. Following target and OARs delineation, virtual reconstruction of tubes was done and plan was generated for the prescribed dose. Treatment was prescribed at a depth of 0.5 cm and the plan was optimized so that the CTV gets coverage of 90% of the dose. The median target volume was 18.45 cc (range: 1.56-40.1 cc). Dose was prescribed at 0.5cm. The median dose at the skin surface was 129.5%. The median V90, and V100 values (or, the volume of the target volume receiving 90%, 100% of the prescribed dose) were 95.3%, 85.6%, respectively. Plan was evaluated and treatment was done by Nucletron Microselectron HDR Afterloader (Ir-192) eighteen channels. Reproducibility of patient’s position was ensured during all fractions.
Results
We followed up the patients at 1st, 3rd, 6th month and then yearly thereafter. Among all the ten cases there were two local recurrences (skin malignancies), one at six months and other at ten months. Two cases died of metastatic disease (recurrent cancer of breast and penile cancer). One case died due to unknown cause (locally recurrent breast cancer) within three months of treatment.
Five (four skin malignancies and one penile cancer) were
disease free till last follow up at 2 years. Skin reactions of grade 2 and 3 were reported during treatment which subsided after 2 to 3 weeks of treatment.
Case 1
76-year-old male (ECOG 2) presented with a 4.5 × 3 cm ulcerative lesion on the right nasal ala, with serosanguinous discharge since three years (Figure 1 and 2).
Figure 1. Nasal Carcinoma at Presentation.

Figure 2. Catheter Placement at the Time of Treatment .

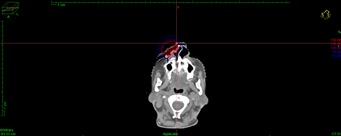
Biopsy confirmed squamous cell carcinoma, and CT imaging showed a 3 × 2 cm lesion without nodal involvement. The patient was treated with HDR mould brachytherapy (51 Gy in 17 fractions, 3 Gy per fraction, on alternate days) (Figure 3).
Figure 3. Axial View of the Treatment Area.
Grade 2 skin reactions developed during treatment but resolved within two weeks after treatment. At 2-year follow-up, no recurrence was observed, and cosmesis was rated as excellent (Figure 4).
Figure 4. Cosmesis Post Treatment.

Case 2
35 yr old women presented with complaints of palpable mass (6 x 6 cm) in lower inner quadrant of right breast. She had skin changes (peaud’orange), retracted nipple with discharge and right axillary lymphadenopathy (4 x 3 cm). Histopathology showed Infiltrating ductal carcinoma and immunohistochemistry resulted in Luminal type A breast carcinoma. Initially she received 4cycle neoadjuvant AC (anthracycline and cyclophosphamide) chemotherapy followed by right breast modified radical mastectomy. Postoperatively she received four cycle adjuvant taxanes, loco-regional external beam radiotherapy (40Gy in 15fractions). After 1 year of Tamoxifen she was switched to Letrozole 2.5 mg once a day. After 3 years on Letrozole she developed solitary chest wall subcutaneous nodule, which was FNAC positive for malignancy. Metastatic work up was done which showed no any other evidence of disease.
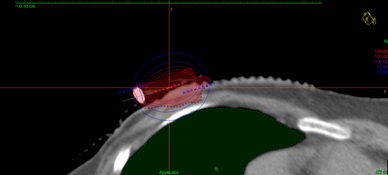
She received SMB to right chest wall nodule, 40Gy in 10 fractions, 4Gy per fraction on alternate days, 3fractions per week (Figure 5, 6).
Figure 5. Placement of the Mould at the Time of Simulation .

Figure 6. Dwell Position of the Source at the Time of Planning.
Chemotherapy was denied by the patient so hormonal treatment was continued.
Locally she was free of recurrence at three and six months. Post 6 months of radiotherapy she developed liver and lung metastases and died after 1 month.
Case 3
A 50 years old male presented with complaints of ulcerative lesion (1.5 x 1 cm) over glans penis with no inguinal lymphadenopathy since 6 months. The patient had no known comorbidities and prepuce was excised 3 years back for infection.
Histopathological examination suggested of well differentiated squamous cell carcinoma of penis. Metastatic work up was normal with no inguinal or retroperitoneal lymphadenopathy, but he had right sided hydrocoele (cT1N0M0).
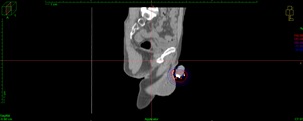
He received SMB for a dose of 32Gy in 10 fractions, 3.2Gy two times a day with minimum 6 hour gap by HDR brachytherapy technique (Figure 7 and 8).
Figure 7. Axial View of Treatment Plan.
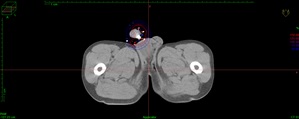
Figure 8. Saggital View of Treatment Plan.
Patient developed grade 2 reactions during radiotherapy and grade 3 reactions after 1 week of completion of radiotherapy. Reactions settled post 3 weeks of brachytherapy. Post one month he was operated for hydrocoele. Now the patient has been five years of follow up with no evidence of disease, no significant late effects and excellent organ preservation.
Discussion
Brachytherapy is the most conformal form of radiotherapy with sharp dose fall off and minimal dose to adjacent structures. Superficial brachytherapy is a useful non-invasive technique for treatment of superficial malignancies. It also gives good cosmesis, good control rates and also organ preservation resulting in better functional outcomes. We reviewed our institutional experience with this technique and reporting three different types of cases out of ten cases.
Surgery is often considered the primary treatment for NMSCs (non-melanoma skin cancers), but often this may not be the best option, due to tumor location (and thus, cosmetic outcomes) or patient comorbidities. Mohs microsurgery has certain limitations with high chances of failure if tumor shows multicentricity, disconnected foci, or satellite lesions [2]. External beam radiotherapy is a useful technique where patient status, comorbidities or tumor location precludes resection, but it can have an impact on adjacent normal structures, resulting in toxicity or cosmetic changes, located within the radiation field. There is evidence suggesting similar rates of local control, late toxicity and cosmetic effects with brachytherapy as compared with EBRT. Delishaj et al. noted in their literature review of ten studies of non melanoma skin cancers treated by HDR brachytherapy. They used the RTOG/EORTC toxicity grading criteria to grade cosmesis into excellent, good, fair and poor category. Patients had excellent cosmetic results in 62% of cases, good results in 26% and poor results in 5.5% [16]. Many of the studies are small and often retrospective, hence GECESTRO’s have given grade B recommendation for the technique (moderate/strong evidence for efficacy but with limitedclinical benefit - generally recommended) [17]. The largest study was performed by Gauden et al. where they prospectively followed 200 patients with 236 skin lesions treated with 36 Gy in 12 fractions using surface brachytherapy. Patients were evaluated regularly for toxicity and cosmetic results, and the LC was 98% (232/236) with a median follow-up of seven months. Four patients developed local recurrences and were salvaged with surgery. Moderate toxicity was noted and 88% of the patients had good/excellent cosmesis. Treatment was completed by all patients and LC was comparable to EBRT patients [10]. Various other retrospective studies have shown similar results with LC varying from 83.3% to as much as 100%. The papers reported variable levels of follow-up, cosmetic results and toxicities [13-18]. In a study by Rio et al. 97 skincarcinomas (88 BCC, 9 SCC) of the nose, periorbital areas, divided in two groups, 40 previously untreated patients (group 1) and 57 patients who had undergone surgery (group 2) were retrospectively analysed. The local control was 92.5% in group 1 and 88% in group 2 (median follow-up 55 months). The average dose was 55 Gy (range: 50–65 Gy) in group 1 and 52 Gy (range: 50–60 Gy) in group 2. Brachytherapy provided good local control and cosmetic results for facial, peri-orificial skin carcinomas that pose problems of surgical reconstruction [19]. Our case 1 and 3 reported control rate of 100% at 2years with good cosmesis. We found no significant toxicities and treatment was well tolerated.
In primary breast cancer role of interstitial brachytherapy is well established [20] but in metastatic case setting role of surface brachytherapy is very less explored. Inerstitial Brachytherapy in metastatic disease has been widely used for spinal metastasis and liver metastasis. Gordon Mao et al summarized the results of various primary and metastatic spinal tumors treated by various brachytherapy modalities and reported recurrence rates of 18-27% across various studies [21]. Case 2 was a post treated carcinoma breast with solitary chest wall recurrence. Control rate was 100% at three months and six months. At seven months patient developed metastatic lung and liver disease but local site was well controlled.
Our case 3 deals with early stage carcinoma penis. Carcinoma penis brachytherapy is well explored. Penile brachytherapy is challenging due to applicator placement reproducibility, immobilization, and the need to treat to appropriate depth although adhering to skin constraints. Interstitial techniques have been mainly used to achieve adequate dose coverage at depth although coupling the applicators to the target site [22]. Hugh et al described a custom mould for treating superficial tumors delivering 40Gy in 10 fractions [22]. In a metanalysis by Shakir Hasan et al total of 2178 males, median age 61 years, were included. 1505 patients in surgery group, and 673 patients in brachytherapy group. Penectomy was associated with a higher 5-year LC rate of 84% compared with 79% with brachytherapy, odds ratio = 1.45 (1.09–1.92, p = 0.009). The 5-year OS with surgery was 76% compared with 73% with brachytherapy, odds ratio = 1.17 (0.95–1.44, p = 0.128). The organ preservation rate for brachytherapy treatment was 74%. Among the surgery patients in a Stage I/II subset, the 5-year OS and LC was 80% (n = 659) and 86% (n = 390), respectively. Of the 209 early stage patients who received brachytherapy, the 5-year OS was 79% and LC was 84%. Chi-square testing demonstrated no difference for either OS or LC for early stage disease [23].
In our case 3 the maximum acute toxicity was grade 3, with no urethral stricture or any late toxicity.It was well controlled at 2 years with 100% local control and no recurrence at 5 years with good organ function.
In conclusion, surface mould brachytherapy is a safe, effective modality for treatment of skin malignancies especially involving challenging sites like nose, eyes, etc. Brachytherapy is overall well tolerated, with no grade 4-5 acute or late toxicities. This treatment is a good alternative option for those patients unwilling or unable to undergo surgery for their superficial malignancies and also can be the primary modality for carefully selected cases. Brachtherapy in metastatic cancers need to be explored more in terms of patient selection and optimal dosing. Brachytherapy is an established alternative in superficial penile tumors with good local control and organ preservation.
Additional Information Disclosures
Human subjects: Consent was obtained by all participants in this study. Animal subjects: All authors haveconfirmed that this study did not involve animal subjects or tissue.
Conflicts of interest
In compliancewith the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info
All authors have declared that no financial support was received from any organization for the submitted work.
References
- Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL , Soerjomataram I, Jemal A. CA: a cancer journal for clinicians.2024;74(3). CrossRef
- Seven years' experience of Mohs micrographic surgery in a UK centre, and development of a UK minimum dataset and audit standards Macfarlane L., Waters A., Evans A., Affleck A., Fleming C.. Clinical and Experimental Dermatology.2013;38(3). CrossRef
- The use of brachytherapy in the treatment of nonmelanoma skin cancer: a review Alam M, Nanda S, Mittal BB , Kim NA , Yoo S. Journal of the American Academy of Dermatology.2011;65(2). CrossRef
- Treatments of Primary Basal Cell Carcinoma of the Skin: A Systematic Review and Network Meta-analysis Drucker AM , Adam GP , Rofeberg V, Gazula A, Smith B, Moustafa F, Weinstock MA , Trikalinos TA . Annals of Internal Medicine.2018;169(7). CrossRef
- High-dose-rate brachytherapy in treatment of non-melanoma skin cancer of head and neck region: preliminary results of a prospective single institution study Kalaghchi B, Esmati E, Ghalehtaki R, Gomar M, Jaberi R, Gholami S, Babaloui S, et al . Journal of Contemporary Brachytherapy.2018;10(2). CrossRef
- High-dose-rate (HDR) plesiotherapy with custom-made moulds for the treatment of non-melanoma skin cancer Montero A, Hernanz R, Capuz A, Fernández E, Hervás A, Colmenares R, Polo A, Sancho S, et al . Clinical & Translational Oncology: Official Publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico.2009;11(11). CrossRef
- Hypofractionated high-dose-rate plesiotherapy in nonmelanoma skin cancer treatment Arenas M, Arguís M, Díez-Presa L, Henríquez I, Murcia-Mejía M, Gascón M, Gómez D, et al . Brachytherapy.2015;14(6). CrossRef
- High dose rate brachytherapy with customized applicators for malignant facial skin lesions Jumeau R., Renard-Oldrini S., Courrech F., Buchheit I., Oldrini G., Vogin G., Peiffert D.. Cancer Radiotherapie: Journal De La Societe Francaise De Radiotherapie Oncologique.2016;20(5). CrossRef
- Hand function after high dose rate brachytherapy for squamous cell carcinoma of the skin of the hand Somanchi B. V., Stanton A., Webb M., Loncaster J., Allan E., Muir L. T. S. W.. Clinical Oncology (Royal College of Radiologists (Great Britain)).2008;20(9). CrossRef
- HDR brachytherapy for superficial non-melanoma skin cancers Gauden R, Pracy M, Avery A, Hodgetts I, Gauden S. Journal of Medical Imaging and Radiation Oncology.2013;57(2). CrossRef
- High dose rate brachytherapy with surface applicators: Treatment for nonmelanomatous skin cancer Musmacher J., Ghaly M., Satchwill K.. Journal of Clinical Oncology.2006;24(18_suppl). CrossRef
- Brachytherapy in non melanoma skin cancer of eyelid: a systematic review Frakulli R, Galuppi A, Cammelli S, Macchia G, Cima S, Gambacorta MA , et al . Journal of Contemporary Brachytherapy.2015;7(6). CrossRef
- HDR Brachytherapy with Standardized Surface Applicators in the Treatment of Superficial Malignant Skin Lesions Ghaly M, Zinkin H, Dannenberg M, et al . ResearchGate.2024. CrossRef
- Non-melanoma skin cancer treated with HDR Valencia applicator: clinical outcomes Tormo A, Celada F, Rodriguez S, Botella R, Ballesta A, Kasper M, Ouhib Z, Santos M, Perez-Calatayud J. Journal of Contemporary Brachytherapy.2014;6(2). CrossRef
- High dose-rate microselectron molds in the treatment of skin tumors Svoboda V. H., Kovarik J., Morris F.. International Journal of Radiation Oncology, Biology, Physics.1995;31(4). CrossRef
- Non-melanoma skin cancer treated with high-dose-rate brachytherapy: a review of literature Delishaj D, Rembielak A, Manfredi B, Ursino S, Pasqualetti F, Laliscia C, Orlandi F, et al . Journal of Contemporary Brachytherapy.2016;8(6). CrossRef
- GEC-ESTRO ACROP recommendations in skin brachytherapy Guinot JL , Rembielak A, Perez-Calatayud J, Rodríguez-Villalba S, Skowronek J, Tagliaferri L, Guix B, et al . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2018;126(3). CrossRef
- Mold brachytherapy can be an optional technique for total scalp irradiation Ozyar E, Gurdalli S. International Journal of Radiation Oncology, Biology, Physics.2002;54(4). CrossRef
- Interstitial brachytherapy of periorificial skin carcinomas of the face: a retrospective study of 97 cases Rio E, Bardet E, Ferron C, Peuvrel P, Supiot S, Campion L, De Montreuil CB , Mahe MA , Dreno B. International Journal of Radiation Oncology, Biology, Physics.2005;63(3). CrossRef
- Late side-effects and cosmetic results of accelerated partial breast irradiation with interstitial brachytherapy versus whole-breast irradiation after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: 5-year results of a randomised, controlled, phase 3 trial Polgár C, Ott OJ , Hildebrandt G, Kauer-Dorner D, Knauerhase H, Major T, Lyczek J, et al . The Lancet. Oncology.2017;18(2). CrossRef
- Spinal brachytherapy Mao G, Theodore N. Neuro-Oncology.2022;24(Suppl 6). CrossRef
- Organ sparing treatment for penile cancer using a 3D-printed high-dose-rate brachytherapy applicator Lee HHC , Chiu TD , Hrycushko B, Xiong Z, Hudak S, Woldu S, Mauck R, et al . Brachytherapy.2023;22(5). CrossRef
- The role of brachytherapy in organ preservation for penile cancer: A meta-analysis and review of the literature Hasan S, Francis A, Hagenauer A, Hirsh A, Kaminsky D, Traughber B, Abouassaly R, Ellis R. Brachytherapy.2015;14(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2025
Author Details