Preventable Risk Factors: Retrospective Analysis of a Cohort of 21 Cases of Cervical Low-Grade Squamous Intraepithelial Lesions
Download
Abstract
Objective: In 2020 we had reported that with non-invasive integrative management, 20 out of 21 cases of Low-grade Intraepithelial Squamous Lesions (LSIL) of cervix responded, whilst one case discontinued early. Subsequent to the analysis by Global Collaborative Group on Cancer Risk Factors in 2022, we report retrospective analysis of Preventable Risk Factors (PRFs) in this cohort.
Materials and Methods: We graded each PRF from 0 to 3 scores as per the severity with grade 0=no risk, 1=minor risk, 2= moderate risk and 3= definite risk. Sixteen PRFs for cervical cancer were scored in all cases into 4 grades. The treated 20 cases were classified in 3 groups according to Pap smear changes- Group 1: persistent LSIL/non-responders (n=2); Group 2: regression to Atypia (n=9); Group 3: responders/regression to negative smears (n=9).
Results: Single or multiple PRFs, other than LSIL in Pap smear at enrolment, were present in every case. Some common PRFs in this cohort were cervico-vaginal infection (21/21), overweight/obesity (11/21), Unhealthy diet (3/21), raised serum IL-6 (3/21) etc. The mean±SD total risk score after grading in Group 1 was 14.5±3.53 vs 10.44±4.66 in Group 2 vs 10.62±1.22 in Group 3.
Mann Whitney U test: p value = 0.051 indicated a nonsignificant trend towards higher risk scores in Group 1 vs Group 3.
Conclusion: All LSIL cases had single or multiple risk factors at initial examination. The total scores of graded PRFs were slightly higher in the persistent LSIL group than in treatment responders, just short of statistical significance. It may be difficult to screen and advise all women to reduce PRFs due to unmanageable numbers. Therefore, at least all screen positive cases should be advised on possible consequences of PRFs. Downgrading PRFs may reduce recurrences and progression to invasive cancer. Some PRFs are common to other cancers and non-communicable diseases hence there are multiple health benefits of such a policy.
Introduction
The dissemination of data analysis of Preventable Risk Factors (PRFs) for cancers in 2022 by Cancer Risk Factors Collaborators, Global Burden of Diseases 2019, has opened up a novel ancillary path for cancer prevention [1]. There is a significant burden of cancers attributable to risk factors and the associated Preventable Risk Factors (PRFs) have been analysed for many cancers. Apart from primary prevention, by methods like antiviral vaccines and occupational safety against carcinogens, secondary prevention by treatment of precancerous lesions detected during screening programs is being adopted extensively, especially for cervical cancer. Precancerous lesions like Squamous Intraepithelial Lesions (SILs) or Cervical Intraepithelial Neoplasia (CIN) can be detected by non-invasive screening methods like Papanicolaou (Pap) smear or colposcopy. Therefore, it may also be possible to reduce cancers by managing PRFs which act as co-factors during carcinogenesis in screen positive cases.
Cervical cancer can be prevented primarily by safe sex habits or by vaccination against Human Papilloma Virus (HPV) i.e. the High Risk or HRHPV oncogenic types, in pubertal period. Vaccination is highly effective when given both to girls and boys in a community [2]. Unfortunately, due to the high costs and other regional factors, vaccination is not uniformly accepted by many countries. The Indian government accepted the policy only in 2023 and due to the availability of indigenous HPV vaccine it is gradually being implemented from 2024 in many states [3]. Nevertheless, already thousands of women in India are HPV positive with estimates of 5% in general population, and higher rates i.e. >30% in some hospital settings in states with high prevalence of invasive cervical cancer [4, 5]. Therefore, there is a prime need for secondary prevention by treatment of precancer lesions. Gynecologists all over India have already initiated both HPV vaccination, as well as secondary prevention by treatment of SILs, on a large scale in many Indian states. Currently, the preferred option for secondary prevention and often the only method utilised by majority of gynaecologists in India, is surgical ablation by surgery, laser ablation, electrocauterization or cryotherapy [6].
In India, there is a large population which is served by traditional practitioners in clinics or in hospital settings. Although they participate in national programs for immunization or other national schemes, some of these facilities have yet not adopted the routine programs for cervical cancer screening or for treatment of precancer lesions. Patients attending these hospitals are free to attend another conventional hospital but most patients may fail to get the benefits of cervical cancer screening programs or treatment of SILs. Especially for the benefit of this population in an Ayurvedic general hospital in Mumbai, we have initiated a collaborative cervical cancer screening and prevention program since 1999. The Ayurvedic gynecologists were willing to collaborate in integrative management and research in leucorrhoea and cervical precancer in women above 25 years of age.
Turmeric extracts are routinely used in Traditional Ayurvedic medicine for management of various ailments like dyspepsia, arthritis, diabetes, skin allergies, wound healing etc. There is considerable experimental data from in vitro, and in vivo studies, apart from clinical experience of traditional practitioners, and recently from some well-designed clinical studies, which supports anticancer and anti-inflammatory activity and safety of standardised turmeric extracts and biomolecules like curcumin. It is known that these standardised medicinal plant extracts have remarkable anti-inflammatory, anti-oxidant, antiproliferative and antiangiogenic properties and are safe for clinical use provided they are well standardised [7-12]. We have recently reported a clinical study on non-invasive integrative management of women, with abnormal Pap smears and persistent LSIL in Pap smear. Integrative treatment consisted of antimicrobials, to control associated genital infections, followed by standardised oral turmeric extract for 10 weeks [11]. Arrest or regression of LSIL as in Pap smears and clinical and biochemical safety of integrative treatment was reported. The study was approved by Ethics Committee and was registered with Clinical Trail Registry of India (CTRI).
Rationale of the present retrospective analysis
The above-mentioned study on non-invasive integrative treatment of LSIL clinical study had i) regression in Pap smears and colposcopy as end points for evaluation of efficacy and ii) clinical and biochemical examinations as end points for safety evaluation. When associated medical conditions, or obesity or reproductive tract infections or high blood sugar were recorded in history and examination, the patients were treated or counselled before participation and were managed as associated diseases, or referred to appropriate departments if required. We had not recorded the risk factors as PRFs for cancer and not emphasized the long-term objective of reducing cancer risk by reducing PRFs. We had included a small booklet in local languages on leucorrhoea and cervical cancer with known risk factors, such as multiple sexual partners, genital infections, immune deficiency or exposure to tobacco at that time as part of patient counselling. This was read by the participating couples before signing consent forms for the study. However, we had not highlighted and counselled women enrolled for the study about all the PRFs during or at the end of the study. We had concentrated on efficacy and safety markers [11]. In view of the subsequent analysis of global data on PRFs in 2022 and additional information on risk factors specific for cervical cancer, we were inspired to undertake a retrospective analysis of PRFs in this recent cohort of LSIL study participants [1, 13]. The data, case record forms and biochemical results of this clinical study were available in the archives of our centre. This short communication describes the outcome of this retrospective analysis in the cohort of LSIL identified and enrolled for the recent study [11]. As this analysis was retrospective and on an exploratory study, we could not have a control group.
Materials and Methods
All participants (N=21) in the clinical study had given informed written consent for use of anonymised data for present and future research [11]. Their Case Record Forms (CRFs) and biochemistry reports were accessed and re-analysed for the following 16 PRFs, apart from persistent LSIL in Pap smears, and were recorded retrospectively for the initial examination: i) Not vaccinated against HRHPV; ii) Never screened earlier; iii) Abnormal Pap smear in the past; iv) Abnormal glandular cells (AGC) reported in current Pap smear; v) Abnormal colposcopy; vi) Koilocytes in Pap smear; vii) Cervico- vaginal infections- nonspecific, or specific, detected in Pap smear; viii) Overweight/obesity; ix) Exposure to tobacco; x) Promiscuity of either partner; xi) Possible Immune-compromission; xii) High fasting blood sugar; xiii) Mental Stress; xiv) Raised circulating Interleukin (IL-6); xv) Unhealthy diet; xvi) Poor Education.
Risk factors like: a) early age at first coitus, b) multiple sexual partners, c) per capita income, d) male circumcision, e) alcohol consumption, were not available in records as we presumed that these may not be common in this cohort, and also that accurate information may not be given by participants. Hence, these risk factors could not be analysed.
Sixteen PRFs for cervical cancer were qualitatively graded in 21 cases at enrolment into 3 grades: Grade 1 = Nil, Grade 2 = minor risk, Grade 3 = definite risk as per review of literature [1, 13]. The treated 20 cases were classified in 3 groups according to Pap smear response to integrative treatment- Group 1: persistent LSIL/non-responders (n=2); Group 2: regression to Atypia (n=9); Group 3: responders/regression to negative smears (n=9).
Statistical methods
Since the sample size in all groups was small and there was no control group, the non-parametric Mann Whitney U test was used to analyse differences between responders and non-responders. Descriptive statistics were used to calculate the mean and standard deviation. The total of all 16 risk factors scores after grading was also calculated for individual cases. The SPSS version 27 was used to analyse the data.
Results
Summary of previous results
Earlier report included regression of LSIL in Pap smear and/or colposcopy in response to treatment along with clinical and biochemical safety markers. Apart from that, mitigation of micrometric features like nucleocytoplasmic ratio, coarse chromatin, and a trend towards decrease in serum IL-6 was reported [11]. Sociodemographic data showed that all cases belonged to low or low-middle income group. Their mean age was 38.19 years (range: 30-48yrs), mean parity was 2.14 (range: 1-3). All were protected against pregnancy. Only 3 out of 21 were graduates, 2 were illiterate, and the rest had primary education.
Retrospectively analysed prevalence of PRFs
The 16 PRFs in this cohort are depicted in Figure 1.
Figure 1. Frequency of Preventable Risk Factors. Abbreviations, HRHPV, High risk Human Papilloma Virus; LSIL, Low-grade Squamous Intraepithelial lesion; RTIs, Reproductive Tract Infections; FBS, Fasting Blood Sugar; AGC, Atypical Glandular Cells. * 6 in treated cases: 1 had discontinued [12].
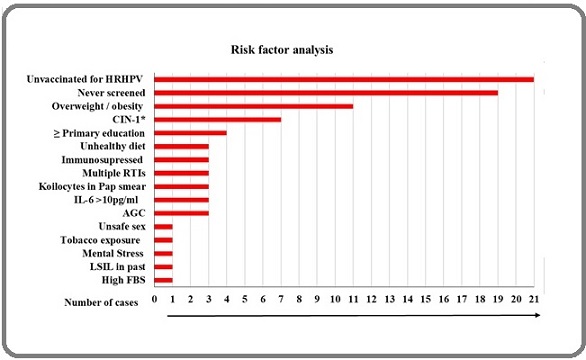
This shows that none of the women were vaccinated and19 had never been screened prior to the study. Common PRFs in this cohort were cervico-vaginal infections, nonspecific - 21/21, and specific 3/21; overweight/obesity-11/21; CIN 1 in colposcopy - 7/21; unhealthy diet - 3/21; raised serum IL-6 -3/21; and AGC- 3/21. The mean total risk score and standard deviation of 16 PRFs after grading in Group 1 was 14.5±3.53 vs 10.44±4.66 in Group 2 vs 10.62±1.22 in Group 3. The mean total risk score and standard deviation of 16 PRFs after grading in Group 1 (Non responders) was 14.5±3.53 vs Group 2 + Group 3 (responders) was 10.56±3.31.
Other common PRFs were poor educational status, Koilocytes in Pap smear, and multiple RTIs.
As depicted in the figure other risk factors were present but in smaller number of cases (<3).
Multiple risk factors (3 or more) were observed in 15 cases.
When we correlated these cases with outcome of treatment for 10 weeks it was observed that the 2 cases of persistent LSIL had > 3 risk factors. Both cases also were in the obese (BMI>30) category (Grade 3) [11].
Statistical analysis: The Mann-Whitney U test was applied to analyse differences between non responders, partial responders and responders (Group 1 vs Group 2 vs Group 3). The p value for Group 1 vs Group 2 was 0.054. The p value for Group 1 vs Group 3 was 0.051 indicating a nonsignificant trend towards higher risk scores in Group 1 vs Group 3.
Discussion
We have reanalysed the data in a cohort of previously reported LSIL cases. In the retrospective analysis we observed that several PRFs were present in this cohort when the new global data on PRFs which has emerged is considered [1, 13]. We had missed out on counselling the screen positive cases about all these PRFs. Out of the 16 factors mentioned above we had warned women only about regular 6 monthly follow up, colposcopic CIN, genital infections, and tobacco exposure in relation to cancer prevention. Obesity and high fasting blood sugar were emphasized from the view point of general health and noncommunicable diseases and not for arrest or regression of carcinogenesis.
We recommend the identification of all these PRFs especially when precancerous changes are observed during screening for cervical cancer. Whilst it may be difficult to carry out identification of PRFs in general community, in camps or in all hospital attendees due to unmanageable numbers, we suggest that these should be identified at least in screen positive cases and given due attention.
The recent research and global PRFs analysis have equipped us with an additional mode of reducing the risk of cancer. Only a small fraction of HRHPV positive women develop cancer [14]. Some recent experimental and epidemiological work on some PRFs is recapitulated for readers participating in screening programs:
i) Adult vaccination against HPV: It is now known that even healthy adult women and HIV positive women can benefit from vaccination against HRHPV [15]. If they are HPV positive for one type of HPV, vaccination against other types can still achieve some protection, though to a lesser degree as the immune response is not as strong as in puberty. It is not necessary to know the HPV status before vaccination but we must warn them that the immune response is suboptimal in adult women and currently available vaccines in public health programs can protect only against 70% of cervical cancers.
ii) Obesity is a preventable risk factor for cervical cancer mortality and possibly for development of adenocarcinoma of cervix [16]. Sociodemographic factors may also be responsible for reduced screening in obese women. Several mechanisms have been revealed which explain how obesity may contribute to carcinogenesis. Eg. Adipocytes may release proinflammatory cytokines in circulation eg. IL-6.
iii) High Fasting Blood Sugar as a risk factor: Fasting blood sugar level (>200 mg%) was associated with increased prevalence and mortality of many cancers [1]. In view of high circulating levels of insulin-like growth factor-1 and insulin-like growth factor binding protein-3 in women with cervical neoplasia it is postulated that prediabetes may also be associated with cervical neoplasia [17].
iv) IL-6: High serum values of IL-6, in cervical neoplasia have been reported in several studies. In both our previous studies on cervical LSIL cases with integrated management we were able to show a reduction in circulating IL-6 levels possibly due to reduced inflammation and regression in the Pap smears [10, 12].
v) AGC reported in Pap smear: AGC reported in 2 cases in Pap smear reports, in initial and follow up smears but we did not emphasize the analysis for AGC only in the initial trial report as we had concentrated only on squamous cell abnormalities [12]. Nevertheless, it is known that HPV infections may also cause adenocarcinomas of cervix although less common.
vi) Cervicovaginal infections: In this cohort, all cases had inflammation reported in Pap smears and in 3 cases specific infections like HPV (Koilocytosis), Chlamydiasis (eosinophilic granules in intracytoplasmic vacuoles) and Bacterial Vaginitis (Clue cells, and absence of Lactobacilli) were reported cytologically in the Pap smear.
Specific tests for different RTIs were not possible. In our previous experience and in recent studies it is increasingly realised that an abnormal vaginal microbiome with anaerobic micro-environment is a co-factor for cervical cancer [18, 19].
Low levels of education, poor socioeconomic status, poor hygiene are typical co-factors or contributary factors for genital infections, cervical neoplasia and cancer, and also to many other diseases in Low & Middle Income Countries. In our study poor educational levels were observed but these do not reflect overall educational levels of residents of Mumbai. A large proportion of patients attending this hospital is from transient migrant families looking for job opportunities. There is a need to specially provide health education related to these risk factors in screen positive women in our setting. In a recent analysis of 50 studies on risk factors for cervical cancer some PRF have been reported [20]. Some risk factors are common to the findings in our report, but we could not report on other risk factors like HIV positivity or immunosuppressive conditions because of our exclusion criteria and a limited sample size in our study.
Although it is ideal to inform all women of these preventable risk factors it seems to be a humongous task when the population at risk in India is considered. But this can be targeted at least in women who are screen positive during cervical cancer screening programs. Hence, counselling screen positive women regarding PRFs may be an added intervention to our attempts at eliminating cervical cancer.
Lastly but not of lesser importance is the fact that these PRFs are also known to contribute to other cancers and NCDs like Diabetes, chronic arthritis, and other age-related degenerative diseases and this additional benefit can improve compliance with preventive measures.
Acknowledgements
We thank Dr Apurva Halbe for her assistance in using the statistical software. We acknowledge the infrastructure support by KHS-MRC for this study.
Funding for project
Nil- Investigator initiated retrospective analysis.
Declarations
Preliminary analysis was presented in National Session of Association of Medical Women of India (AMWI) Conference in Mumbai on 24th November, 2024 and received 1st prize.
Ethics approval and consent to participate
Not applicable.
Conflict of Interest
Nil
References
- The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019 GBD 2019 Cancer Risk Factors Collaborators . Lancet (London, England).2022;400(10352). CrossRef
- The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study Falcaro M, Castañon A, Ndlela B, Checchi M, Soldan K, Lopez-Bernal J, Elliss-Brookes L, Sasieni P. Lancet (London, England).2021;398(10316). CrossRef
- India rolls out HPV vaccination Burki TK . The Lancet. Oncology.2023;24(4). CrossRef
- ICO/IARC Information Centre on HPV and Cancer India. Human Papilloma virus and Related Cancers, Fact Sheet 2023 (2023-03-10)..
- Prevalence, risk factors and genotype distribution of human papillomavirus infection among women with and without invasive cervical cancer: Findings from a hospital-based study in Bihar, India Pankaj S, Rani J, Kumari P, Abhilashi K, Choudhary V, Kumari S, Shahi SK , Jee B. The National Medical Journal of India.2024;37(1). CrossRef
- Cervical Cancer: Formulation and Implementation of Govt of India Guidelines for Screening and Management Mehrotra R, Yadav K. Indian Journal of Gynecologic Oncology.2022;20(1). CrossRef
- Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions Cheng A. L., Hsu C. H., Lin J. K., Hsu M. M., Ho Y. F., Shen T. S., Ko J. Y., et al . Anticancer Research.2001;21(4B).
- Early human safety study of turmeric oil (Curcuma longa oil) administered orally in healthy volunteers Joshi J, Ghaisas S, Vaidya A, Vaidya R, Kamat D. V., Bhagwat A. N., Bhide S. The Journal of the Association of Physicians of India.2003;51.
- Chemopreventive potential and safety profile of a Curcuma longa extract in women with cervical low-grade squamous intraepithelial neoplasia Joshi J. V., Paradkar P. H., Jagtap S. S., Agashe S. V., Soman G., Vaidya A. B.. Asian Pacific journal of cancer prevention: APJCP.2011;12(12).
- Assessment of in vitro - in vivo antimigratory and anti-angiogenic activity of Curcuma longa linn. and Tinospora cordifolia Willd. Extracts in cervical cancer Paradkar PH , Dandekar SP , Joshi JV , Amonkar AJ , Vaidya AB . International Journal of Pharmacology, Scientific Review & Research.2017;42:87-93.
- Integrated Non-invasive Management of Cervical Low-Grade Squamous Intraepithelial Lesions Observed in Papanicolaou Smears with Antimicrobials Followed by Oral Curcuma Longa Extract Joshi JV, , Jagtap SS , Rastogi N, Walwatkar P, Nabar NS , Hingorani L. ResearchGate.2024. CrossRef
- Role of Turmeric and Curcumin in Prevention and Treatment of Chronic Diseases: Lessons Learned from Clinical Trials Kunnumakkara AB , Hegde M, Parama D, Girisa S, Kumar A, Daimary UD , Garodia P, et al . ACS pharmacology & translational science.2023;6(4). CrossRef
- Global distribution, risk factors, and recent trends for cervical cancer: A worldwide country-level analysis Huang J, Deng Y, Boakye D, Tin MS , Lok V, Zhang L, Lucero-Prisno DE , et al . Gynecologic Oncology.2022;164(1). CrossRef
- Long-term absolute risk of cervical intraepithelial neoplasia grade 3 or worse following human papillomavirus infection: role of persistence Kjær SK , Frederiksen K, Munk C, Iftner T. Journal of the National Cancer Institute.2010;102(19). CrossRef
- Concomitant human papillomavirus (HPV) vaccination and screening for elimination of HPV and cervical cancer Arroyo Mühr LS , Gini A, Yilmaz E, Hassan SS , Lagheden C, Hultin E, Garcia Serrano A, et al . Nature Communications.2024;15(1). CrossRef
- Obesity and Cancer: A Current Overview of Epidemiology, Pathogenesis, Outcomes, and Management Pati S, Irfan W, Jameel A, Ahmed S, Shahid RK . Cancers.2023;15(2). CrossRef
- Plasma levels of insulin-like growth factor-1 and insulin-like growth factor binding protein-3 in women with cervical neoplasia Lee SW , Lee SY , Lee SR , Ju W, Kim SC . Journal of Gynecologic Oncology.2010;21(3). CrossRef
- The association of cervical intraepithelial neoplasias and sexually transmitted diseases in Papanicolaou smears (correlation with cervical biopsy in a subset) Joshi JV , Mali BN , Hazari K , Shah RS , Chitlange SC . Journal of Vivekananda Institute of Medical Sciences.1994;17:9-13.
- The interplay between human papillomavirus and vaginal microbiota in cervical cancer development Sharifian K, Shoja Z, Jalilvand S. Virology Journal.2023;20(1). CrossRef
- Risk factors for human papillomavirus infection, cervical intraepithelial neoplasia and cervical cancer: an umbrella review and follow-up Mendelian randomisation studies Bowden SJ , Doulgeraki T, Bouras E, Markozannes G, Athanasiou A, Grout-Smith H, Kechagias KS , et al . BMC medicine.2023;21(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2025
Author Details