A Metastatic Papillary Thyroid Carcinoma Could be Confused Clinically with a Primary Renal Neoplasm; A Case Report and Literature Review
Download
Abstract
Background: Papillary thyroid carcinoma is the most common thyroid neoplasm. It has a very high incidence of regional lymph node metastasis at the initial presentation. However, vascular spread is a very uncommon event. Lungs and bones are the most frequent sites of vascular metastasis from papillary thyroid carcinoma.
Case concerns: The currently discussed case was obtained from the archive of Pathology laboratory, Sohag University. A 46-year-old female patient admitted to Urology Department, Sohag University, in 2015. The patient had a left loin pain, no other clinical data included in her referral sheet . Radiological findings revealed a renal mass and left radical nephrectomy was performed. Histopathological evaluation revealed a circumscribed neoplasm, formed of densely packed acini with scanty stroma. The patient was diagnosed as renal oncocytoma. On re-evaluation of the Hematoxylin and Eosin-stained slides; the nuclear features were different from those described in renal oncocytomas. So, a panel of immunohistochemical markers was performed (anti-CK7, anti-EMA, anti-Vimentin, anti-Thyroglobulin and anti-TTF1).
Results: The neoplastic cells showed strong and diffuse cytoplasmic expression for Thyroglobulin and CK7 and nuclear expression for TTF1. The neoplastic cells didn’t express EMA or Vimentin. Based on the characteristic nuclear features detected by Hematoxylin and Eosin-stained slides and the obtained immunohistochemical results; the diagnosis of metastatic papillary thyroid carcinoma to the kidney was confirmed.
Conclusions: Papillary thyroid carcinoma may metastasize to the kidney and form a solitary mass, that could be confused as a primary renal neoplasm.
Introduction
Thyroid carcinoma is the most common malignant neoplasm in women and the most common carcinoma affecting women who are younger than 25 years old. Papillary thyroid carcinoma (PTC) is the most common thyroid neoplasm. In 2017; PTC represented about 90% of all diagnosed thyroid cancers, while follicular carcinoma, hűrthle cell carcinoma, medullary and anaplastic carcinomas occupied 4.4%, 1.5%, 1.5% and 1%, respectively [1]. It is very common for PTC to invade the intraglandular lymphatics with very high incidence of regional lymph node metastasis reaching 50% of cases at time of first presentation [2]. However, venous invasion is uncommon, it doesn’t exceed 7% of cases. The most common sites of distant metastasis are lungs and bones [3]. Herein, we reported a case of metastatic PTC in the kidney of a female patient in her fifth decade of life. The case was obtained from the archive of Pathology laboratory, Sohag University, during recruiting formalin-fixed and paraffin-embedded tissue blocks that were previously diagnosed as renal neoplasms.
Case presentation
Patient information and Clinical findings
A 46-year-old female patient admitted to Urology Department, Sohag University, in 2015. The patient suffered from left loin pain for three months. She underwent abdominal ultrasound which detected a left renal mass occupied the upper pole. Therefore, the patient underwent left radical nephrectomy and the specimen was sent to Pathology laboratory. No other clinical data were included in the referral sheet.
Pathological features
The gross features of the specimen, as obtained from the archived pathology report, revealed a non-capsulated, soft and rounded mass occupied the upper pole of the excised kidney. The mass measured about 2.7x3.5x4 cm. it was dark red in color with heterogonous cut section. The mass didn’t invade the attached peri-renal fat.
Microscopic features revealed a non-capsulated, well circumscribed cellular growth, formed of densely packed glands. Some of these glands were cystically dilated and their lumens were filled with homogenous, pale eosinophilic material with occasional peripheral scalloping. The cells that line these glands were cuboidal with moderate amount of pale eosinophilic cytoplasm. The stroma was scanty with few thin walled and ectatic vascular channels (Figure 1).
Figure 1. Microscopic Features of the Lesion which is Non-capsulated but Well Circumscribed from Normal Renal Tissue (a: X 10), the Neoplasm is Formed of Closely Packed Acini with Little Intervening Stroma (b: X 20), the Acini are Filed with Eosinophilic Material with Clear Nuclei (c: X 40).
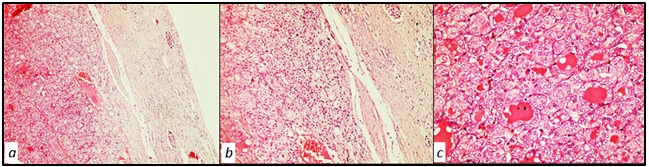
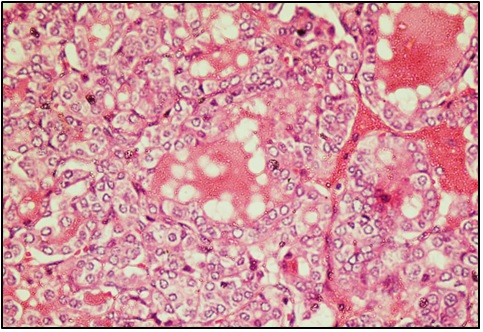
The surrounding renal tissue was unremarkable. These histological findings made the diagnosis of renal oncocytoma is the most appropriate. However. The nuclear features of these neoplastic cells that were ubiquitously present were attractive. On re-evaluating the Hematoxylin and Eosin (H&E)-stained slides, we noticed a nuclear overlapping, the nuclei were large and optically clear with frequent nuclear grooving and indentations (Figure 2).
Figure 2. The Nuclei are Overcrowded, Optically Clear with Irregular Nuclear Membranes and Frequent Nuclear Grooves.
Immunohistochemical study
From the paraffin blocks, multiple 4μm tissue sections were obtained and immunohistochemically stained by antibodies against Thyroglobulin, Thyroid Transcription Factor-1 (TTF-1), Epithelial membrane antigen (EMA), Vimentin and Cytokeratin 7 (CK7).
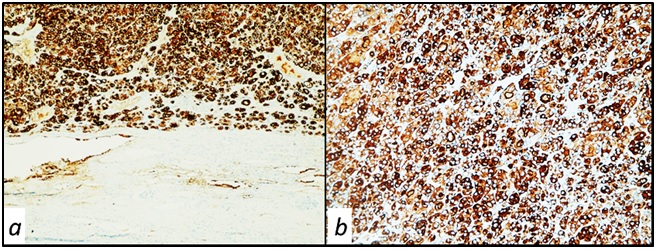
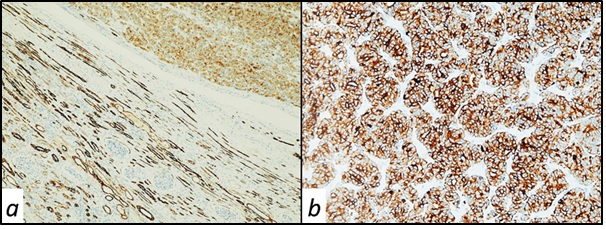
We detected diffuse and strong, cytoplasmic and membranous expression of thyroglobulin in the neoplastic cells (Figure 3).
Figure 3. Diffuse Cytoplasmic Expression of Thyroglobulin in Neoplastic Cells but Not Renal Tissues a: x10, b: X 20.
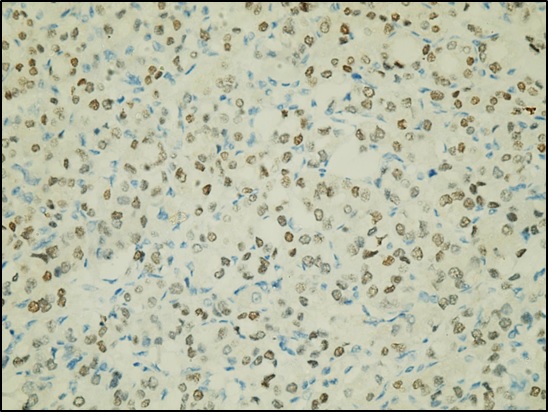
Nuclear expression of TTF1 was detected in the neoplastic glands and acini (Figure 4).
Figure 4. Nuclear Expression of TTF1 in Neoplastic Cells, X 40.
CK7 showed cytoplasmic expression in both neoplastic cells and normal renal tubules (Figure 5).
Figure 5. Cytoplasmic Expression of CK7 in both Neoplastic Cells and Normal Renal Tubules. a: x10, b: X 20.
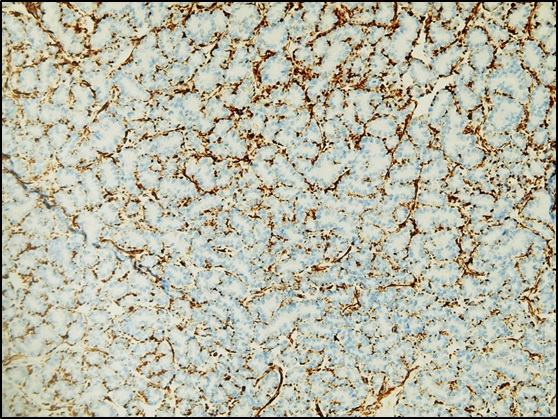
The neoplastic cells didn’t express EMA or Vimentin. EMA was detected in the normal renal tubules (Figure 6), while Vimentin stained the intervening stroma between the neoplastic glands (Figure 7).
Figure 6. Expression of EMA in Normal Renal Tubules but not the Neoplastic Cells, X 20.
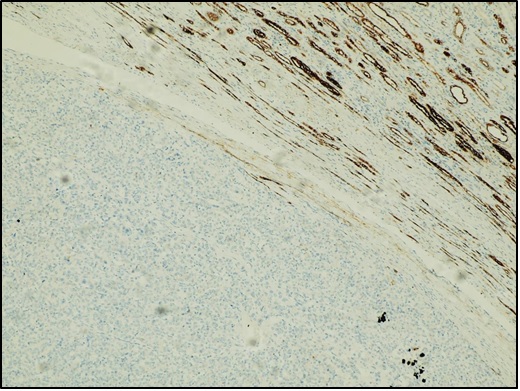
Figure 7. Expression of Vimentin in the Intervening Stroma between the Neoplastic cells, X 20.
Discussion
Malignancy of the thyroid gland is the most common malignant neoplasms of the endocrine system [2]. PTC is the most frequently occurring subtype of thyroid carcinoma, accounting about 90% of all thyroid cancers. It is a well differentiated tumor in the vast majority of cases, which starts as a painless slowly growing nodule [4]. Lymphatic spread to the regional lymph nodes is very common at time of initial diagnosis of PTC. However, such nodal metastasis doesn’t adversely affect the prognosis [2]. Distant spread through blood stream is very uncommon in PTC, and if it occurs, it usually carries a less favorable prognosis [3].
It is very uncommon to find metastatic deposits in the kidney from primary thyroid carcinoma, and most of the reported metastatic cases are usually of follicular subtype. Follicular carcinoma of the thyroid reported in more than 50% of the metastatic thyroid carcinomas to the kidney in previous literatures, while PTC was reported in only 13% of cases [5]. Furthermore, It has been found that intra- renal metastatic deposits from primary thyroid carcinoma usually develops a long time after resection of the thyroid lesion. So, any renal masses could be easily misdiagnosed as a primary renal neoplasm [6].
In our case, a female patient suffered from left loin pain for three months duration. Radiological findings revealed a left upper pole renal mass. Both clinical and radiological data strongly supported a primary renal neoplasm. The gross pathological features were also in favor of a primary renal neoplasm as the mass was solitary and occupied the upper pole of the kidney, which is the most frequent location of primary renal tumors.
Microscopic features were rather confusing. Architecturally; the tumor was circumscribed and formed of densely packed glands and acini with little intervening stroma. A picture reminiscent of renal oncocytoma. However, the nuclear features were different from those of renal oncocytoma, the nuclei were overcrowded and optically clear, frequent nuclear indentations and grooving were seen. Because of the insufficient clinical data in the referral sheet and loss of contact with the patient after her radical nephrectomy, there wasn’t any argument that can be relied upon to explain these nuclear features.
On re-evaluation of the slides; A cocktail of immunohistochemical markers was highly recommended. Tissue sections were stained by anti-CK7, anti-Vimentin, anti-EMA, anti-TTF1 and anti-Thyroglobulin. The neoplastic cells strongly and diffusely expressed CK7. It is well known that renal oncocytoma is negative for CK7 or show patchy distribution [7].
Two other possibilities were highly suggested; thyroid-like follicular variant of renal cell carcinoma (TLFRCC) and a metastatic PTC. The former is a rare primary renal epithelial neoplasm. It was firstly reported in 2006. This neoplasm is positive for renal cell carcinoma markers as EMA, Vimentin and PAX8, while it is strictly negative for thyroid markers as Thyroglobulin and TTF1 [8, 9]. In our case, the tumor cells didn’t express EMA or Vimentin. However, we detected diffuse and strong cytoplasmic and membranous expression of the tumor cells to Thyroglobulin and positive nuclear expression of TTF1 in the neoplastic cells. From the obtained results, the diagnosis of metastatic papillary thyroid carcinoma to the kidney was confirmed.
In conclusion, vascular metastasis from PTC is an uncommon event and if it occurs, it usually reaches lungs and bones. However, kidneys may be sites for blood born spread from PTC. A panel of immunohistochemical markers specific for renal and thyroid tissues may be needed in such suspected cases in order to reach the accurate diagnosis.
Competing interests
The authors declare that they have no competing interests.
Funding
No financial support was received for this study.
Lists of abbreviations
PTC, Papillary Thyroid Carcinoma; H& E, Hematoxylin and Eosin; TTF-1, Thyroid Transcription Factor-1; EMA, Epithelial Membrane Antigen; CK7, Cytokeratin 7; TLFRCC, Thyroid-Like Follicular Variant of Renal Cell Carcinoma.
References
- A worldwide journey of thyroid cancer incidence centred on tumour histology Rossi Esther Diana, Pantanowitz Liron, Hornick Jason L.. The Lancet. Diabetes & Endocrinology.2021;9(4). CrossRef
- Metastatic papillary thyroid carcinoma of the mandible: Case report and literature review Khoozestani Neda Kardouni, Mosavat Farzaneh, Shirkhoda Mohammad, Sedaghati Azin. Journal of oral and maxillofacial pathology: JOMFP.2019;23(Suppl 1). CrossRef
- Renal metastases as the initial presentation of papillary thyroid carcinoma: A case report and literature review Gao Yunfei, Deng Weiye, Chen Yanfeng, Fan Yunping, Guo Zhuming. Molecular and Clinical Oncology.2017;6(6). CrossRef
- Mandibular metastasis revealed papillary thyroid carcinoma: Rare case Anajar Said, Hassnaoui Jawad, Rouadi Sami, Abada Reda, Roubal Mohammed, Mahtar Mohammed. International Journal of Surgery Case Reports.2017;37. CrossRef
- Unusual case of adrenal and renal metastases from papillary carcinoma of thyroid Malhotra Gaurav, Upadhye Trupti S., Sridhar Epari, Asopa Ramesh V., Garde Parul S., Gawde Sachin, Rangarajan Venkatesh. Clinical Nuclear Medicine.2010;35(9). CrossRef
- Unusual Thyroid Carcinoma Metastases: a Case Series and Literature Review Farina Eleonora, Monari Fabio, Tallini Giovanni, Repaci Andrea, Mazzarotto Renzo, Giunchi Francesca, Panzacchi Riccardo, Cammelli Silvia, Padula Gilbert D. A., Deodato Francesco, Pasquali Renato, Fanti Stefano, Fiorentino Michelangelo, Morganti Alessio G.. Endocrine Pathology.2016;27(1). CrossRef
- Cytokeratins 7 and 20 immunoreactivity in chromophobe renal cell carcinomas and renal oncocytomas Wu Sang Ling, Kothari Pulin, Wheeler Thomas M., Reese Tommy, Connelly John H.. Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc.2002;15(7). CrossRef
- Thyroid follicular carcinoma-like renal tumor Zhang Yujie, Yang Jing, Zhang Mingfang, Meng Zhaowei, Song Wenjing, Yang Long, Li Liming, Wang Dan, Shi Tao. Medicine.2018;97(21). CrossRef
- [Clinicopathologic characteristics of thyroid-like follicular carcinoma of the kidney: an analysis of five cases and review of literature] Chen X, Dou F. X, Cheng X. B, Guo A. T, Shi H. Y. Zhonghua bing li xue za zhi = Chinese journal of pathology.2016;45(10). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2022
Author Details