Male Breast Cancer: A Retrospective Analysis of Clinical and Pathological Features at a Tertiary Care Center
Download
Abstract
Background: Male breast cancer is a rare disease, accounting for approximately 0.5-1% of all breast cancer cases. While recent data suggest a slow rise in incidence, epidemiological data on male breast cancer remains limited compared to female breast cancer due to its rarity. The disease typically presents in older men, often in their sixth or seventh decade of life, and is often diagnosed at an advanced stage with a poorer prognosis than female breast cancer. This study aimed to analyze the epidemiological, clinical, and pathological characteristics of male breast cancer patients.
Methods: This retrospective study included 11 male breast cancer patients who presented to the Department of General Surgery at RIMS, Ranchi, over a one-year period. Data regarding clinical history, physical examination findings, family history, disease stage, histopathological examination, and hormonal status were collected and analyzed.
Results: The median age at diagnosis was 58.5 years. The average delay in diagnosis was 6.6 months. Of the 11 patients, eight had left breast involvement, and three had right breast involvement. Invasive ductal carcinoma was the most common histological type, seen in nine cases. Ten patients presented with advanced stage T4 disease, while one presented at stage T3. Hormone receptors were positive in 81.8% of cases.
Conclusion: Male breast cancer is a rare disease with multiple and diverse risk factors. While it shares similarities in clinical, histological, and prognostic features with breast cancer in women, it also exhibits unique characteristics. To promote early diagnosis and improve prognosis, educational efforts should include teaching self-breast examination to men, advocating for screening mammography in high-risk groups, and testing for familial predisposition. Increased public awareness programs are crucial to educate men about breast cancer and encourage early detection.
Introduction
Male breast cancer is a rare disease. It represents only 0.6% of all breast cancers and less than 1% of all causes of male cancer [1]. Male breast cancer is a relatively rare malignancy when compared to female breast cancer (FBC). The ratio of male breast carcinoma to female is 1:100 cases . Incidence is relatively low in men because of presence of less amount of breast tissue. It is also because of the difference in their hormonal environment when compared to female. In the past few decades concern about male breast carcinoma has increased, as the incidence has been rising rapidly. Review of Surveillance, Epidemiology and End Result data (SEER) indicates an [2,3] increased incidence of male breast cancer from 1.0 per 100,000 men in the late 1970s to 1.2 per 100,000 men from 2000 to 2004. Most male breast cancer occurs in elderly men. [4-6]. It is more commonly seen on left side with a ratio of 1.07:1 with respect to right side [7]. Diagnostic and treatment evidence for male breast cancer is limited. Currently, male breast cancer is treated similar to female breast cancer [6,8].
Presentation
The most common presentations are painless palpable mass, skin ulceration, and nipple retraction or discharge in approximately 63 % of the cases, similar to women. As the males have relatively less breast tissue, nipple is mostly involved at early stages in most cases. The incidence of retraction of nipple is around 9%, for discharge it is 6% and ulceration being 6%. The mass is frequently localized to the subareolar region. It is seen less frequently in the upper outer quadrant. The left breast is involved more frequently than the right; 1% of the cases are bilateral. Others include Gynecomastia and Axillary lymphadenopathy (Figure 1-4).
Figure 1. Frontal View of Different Presentations of Patients. a, With nipple environment; b, Without nipple environment; c, Advanced stage cancer.

Figure 2. Frontal View of Specimen Taken after Modified Radical Mastectomy of Left Breast .
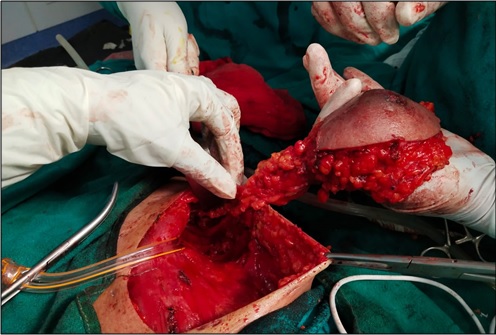
Figure 3. Frontal View of Scar Following Modified Radical Mastectomy Left Breast .

Figure 4. Left Breast Biopsy Positive for Invasive Ductal Carcinoma.

Diagnosis
Diagnosis of male breast cancer is mostly done by triple assessment similar to female breast cancer. Triple assessment which includes clinical assessment, mammography or ultrasonography, and core biopsy. Physical examination includes palpation of breast lump with axillary lymph nodes. The size of the tumour, it’s consistency, boundary and mobility should be assessed. Male breast cancer is usually presents as hard mass, ill-defined margins and which has poor mobility, mostly fixed to breast tissue [9]. Ultrasound and trucut biopsy are routine preoperative examinations for breast cancer. Breast ultrasound shows usually a mass with unclear boundaries, incomplete capsule, and abundant vascular supply [10]. Mammography is difficult to carry out in male patients because of low breast tissue in males. Experienced mammography technicians are required for it if necessary. Mammography in male breast cancer shows high density mass with unclear boundaries and presence of burrs [7]. For most patients, enhanced magnetic resonance imaging is less available than ultrasound and mammography as it is costlier and more time consuming. Magnetic resonance imaging of male breast cancer shows irregular shape and enhanced signal of lesion. Based on all the above examination, we make the diagnosis of male breast cancer in clinic but the final diagnosis is made by histopathological examination.
Risk Factors
Male breast cancer etiology mostly includes the genetic or environmental risk factors. It is important to be mindful when discussing those risk factors in a case of male breast cancer. Majority of males who have been diagnosed with male breast cancer have no identifiable risk other than increasing age (average age of diagnosis of 71 years) [4]. Risk of male breast cancer increases if they have first or second degree relative with breast cancer which is similar to cancer seen in women. Studies have shown that the affected first or second degree relative of either gender may increase the risk of breast cancer in either the males or females in the family.
Along with family history, increased risk for breast cancer in males is seen with BRCA mutation. It is mostly rare for a male to have a BRCA mutation, but those with BRCA2 carrier mutation have a 6% increased risk and BRCA1 carrier mutation have an increased risk of 4% for developing the disease [6]. Other genetic disorders which have been implicated in increasing the risk of male breast cancer includes Klinefelter syndrome (47, XXY), Cowden syndrome (PTEN tumour suppressor gene), Li-Fraumeni syndrome (TP53), Lynch syndrome (PALB2 and mismatch repair genes) [4][6].
The alterations in oestrogen to androgen ratios is important in etiology of male breast cancer and carries an important role. Same as female breast cancer oestrogen, which stimulates ductal development in breasts, has also been implicated as a potential risk factor for male breast cancer. Klinefelter syndrome as previously mentioned, increases the risk of male breast cancer by stimulating excess oestrogen. Other potential triggers include obesity, marijuana use, hepatic dysfunction, thyroid disease, and oestrogen-containing medications [4]. Similarly, a decrease in circulating androgens would result in elevations of the oestrogen, thus causing alteration in oestrogen and androgen ratios, and predisposing to male breast cancer. This alteration is mostly seen in conditions such as cryptorchidism, orchitis, and orchiectomy [8].
Lastly, environmental factors have also been playing an important role for increasing the risk of male breast cancer. In males’ previous radiation therapy has been noted as a potential risk factor like females. Radiation therapy increases the risk of male breast cancer 7 times. In males generally radiotherapy has been used to treat gynecomastia [2]. In addition to all this, certain occupations have also been implicated to increase the risk of MBC, including steel and rolling mills, as well as occupations involved with organic solvents such as trichloroethylene [3].
Aims and Objectives
• To discuss the epidemiological, clinical, and histological features of male breast cancer.
• To discuss the therapeutic management as well as the survival rates and factors of this disease.
Materials and Methods
This work is prospective work of 11 male breast cancer patients who presented in department of general surgery rims Ranchi during a period of 1 year. Data regarding clinical history, examination findings, family history, stage of the disease, histopathological examination and hormonal status were evaluated.
Inclusion Criteria:
a. All male patients admitted in surgical ward through OPD/ Emergency with breast lump or ulcer.
b. Male patients aged more than 18 years. Exclusion Criteria:
a. Patients who succumbed to death during the course of treatment.
b. Study patients who had no follow-up after initial diagnosis.
Variables Studied:
• Age at diagnosis
• Family history
• Tumour size (in cm)
• Grade
• Stage of the tumour
• Histological subtype of the tumour
• Axillary lymph node status
• Average delay in diagnosis
• Oestrogen receptor (ER) expression,
• Treatment
Results
In my study, Male breast cancers occurred later in life with late stage and more ER PR receptor-positive tumours. The Median age being 58.54 years. Family history was found positive in one case. The average Mean diameter of lump was 8.77 cm (range: 3-20 cm) and tumor was predominantly on the left side (72.72%). The Average diagnosis delay for patients was 6.66 months. According to TNM classification 10 patients presented at T4 stage (90.90%) and one patient presented at T3. Axillary nodal involvement was seen in 72.72% of cases. Three patient was Node negative (27.27%) and N1 was seen in 6 cases (54.54%), while N2 was seen in 2 case (18.18%). Histopathological finding was infiltrating ductal carcinoma in 9 cases. (81.8%), One case was ductal carcinoma in situ and one was spindle cell carcinoma. Hormone receptors (ER/PR) was positive in 81.81% cases. Rest patients were not financially supportive for the test. Neoadjuvant chemotherapy with CAF regimen followed by Modified radical mastectomy followed by adjuvant Chemotherapy was given to 7 patients. Neoadjuvant chemotherapy with CAF regimen followed by Modified radical mastectomy and axillary lymph node sampling followed by adjuvant Chemotherapy was given to 2 patients One patient underwent mastectomy and one underwent WLE (Table 1).
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 | Case 11 | ||
| 1 | Age at diagnosis | 68 years | 70 years | 58 years | 60 years | 56 years | 50 years | 57 years | 74 years | 62 years | 20 years | 69 years |
| 2 | Family history | Negative | Negative | Positive | Negative | Negative | Negative | Negative | Negative | negative | Positive | Negative |
| 3 | Mode of presentation | Swelling + | Swelling + | Swelling - | Swelling + | Swelling - | Swelling - | Swelling + | Swelling + | Swelling - | Swelling + | Swelling + |
| Ulceration + | Ulceration + | Ulceration + | Ulceration + | Ulceration + | Ulceration + | Ulceration + | Ulceration + | Ulceration + | Ulceration - | Ulceration + | ||
| Pain - | Pain + | Pain - | Pain - | Pain + | Pain - | Pain - | Pain - | Pain - | Pain - | Pain - | ||
| Nipple distortion or discharge + | Nipple distortion or discharge + | Nipple distortion or discharge + | Nipple distortion or discharge + | Nipple distortion or discharge + | Nipple distortion or discharge + | Nipple distortion or discharge + | Nipple distortion or discharge - | Nipple distortion or discharge + | Nipple distortion or discharge - | Nipple distortion or discharge + | ||
| 4 | Average diagnosis delay | 14 months | 18 months | 5 months | 6 months | 10 months | 7 months | 4 months | 5months | 3months | 2months | 6 months |
| 5 | Tm size (in cm) | 14*18*6 | 20*10*8 | 4*4*3.5 | 7*5*3 | 16*14*8 | 3*2*2 | 7*6*4 | 6*5*3 | 4*3*1.5 | 3.5*2*1.5 | 8*6*4 |
| 6 | Side of tumor | Left | Left | Left | Left | Left | Left | Right | Left | Right | Right | left |
| 7 | Axillary LN status | Positive | Positive | Negative | Positive | Positive | Positive | Positive | Positive | Positive | negative | negative |
| 8 | TNM Stage | T4bN1M0 | T4bN2aM0 | T4bN0M0 | T4BN1M0 | T4bN1M0 | T4bN1M0 | T4BN1M1 | T4BN2aM0 | T4BN1M0 | T3N0M0 | T4BN0M0 |
| 9 | Histological subtype | Ductal | Ductal | Ductal | Ductal | Ductal | Ductal | Ductal | Ductal | Ductal | Ductal carcinoma in situ | Spindle cell carcinoma |
| 10 | Grade | Poorly differentiated | Poorly differentiated | Mod differentiated | Mod differentiated | Poorly differentiated | Well differentiated | Mod differentiated | Mod differentiated | Mod differentiated | Well differentiated | Well differentiated |
| 11 | Stage | IIIB | IIIB | IIIB | IIIB | IIIB | IIIB | IV | IIIB | IIIB | IIIA | IIIB |
| 12 | ER/PR status | ER + | ER + | ER + | ER + | ER + | ER + | ER + | ER + | ER + | Not done | Not Done |
| PR - | PR + | PR + | PR + | PR - | PR + | PR - | PR + | PR + | ||||
| Her 2 neu - | Her 2 neu - | Her 2 neu - | Her 2 neu - | Her 2 neu - | Her 2 neu - | Her 2 neu - | Her 2 neu - | Her 2 neu - | ||||
| 13 | Treatment | Left MRM | Left MRM | Left MRM | Left MRM | Left MRM | Left MRM | Right MRM | Left MRM | Right MRM | Mastectomy | WLE |
| 14 | HPE | Margin not involved | Margin not involved | Margin not involved | Margin not involved | Margin not involved | Margin not involved | Margin not involved | Margin not involved | Margin not involved | Margin not involved | Margin not involved |
| Node involvement present | Node involvement present | Node involvement absent | Node involvement present | Node involvement present | Node involvement present | Node involvement present | Node involvement present | Node involvement present | Node involvement absent | Node involvement absent | ||
| Lymphovascular invasion present | Lymphovascular invasion present | Lymphovascular invasion absent | Lymphovascular invasion absent | Lymphovascular invasion present | Lymphovascular invasion absent | Lymphovascular invasion absent | Lymphovascular invasion absent | Lymphovascular invasion absent | Lymphovascular invasion absent | Lymphovascular invasion absent |
Discussion
The average age of our patients (58.54 years) which is almost similar to study done by A. Sanguinetti et al. (2016) [10] which is 62 years and Chao li and Xujung li et al (2022) which is 60 years. In study done by Majdouline El Fouhi et al (2022) [11] it was slightly higher, that is 67.7 years. Collective reviews have shown predilection for the left side in a ratio of 1.07:1. In our series also more patients had lump on the left side. (72.72%). The average diagnosis delay of our patients was 6.66 months which is slightly lower than that seen in other series, In studies Figure 1. Frontal View of Different Presentations of Patients. a, With nipple environment; b, Without nipple environment; c, Advanced stage cancer done by A. Sanguinetti et al. (2016) [10] it was 16 months and study done by Majdouline El Fouhi et al (2022) [11] it was 15.7 months. 81.8% cases of male breast tumors have turned out to be invasive ductal carcinomas in our study, expressing high levels of hormone receptors. In studies done by A. Sanguinetti et al. (2016) [10], Chao li and Xujung li et al (2022) and Majdouline El Fouhi et al (2022) (11), 95% (45/47), 80.7% (21/26), 92% (23/25) patients had Infiltrating ductal carcinoma (IDC) respectively. All these studies show that infiltrating ductal carcinoma is the most predominant subtype with an incidence ranging from 64-93%. Axillary lymph node involvement is very common and we report a rate of 72.72 % of axillary nodal involvement which is almost similar to study done by A. Sanguinetti et al. (2016) [10]: 79.4% (39/47) and Majdouline El Fouhi et al (2022) [11]: 80% (20/25) but it differed with study done by Chao li and Xujung li et al (2022) which showed 53.84% (14/26) axillary lymph node involvement. Breast cancer in males should be treated with the same strategy in women. The most common surgical procedure is modified radical mastectomy with axillary node dissection In our series, modified radical mastectomy was the common surgical procedure combined with adjuvant chemotherapy. Frequently used chemotherapy regimens were cyclophosphamide adriamycin fluorouracil (CAF). Majority of our patients have recieved the same. In My study Hormonal receptors (both ER and PR) were positive in 54.54% of case and ER was positive in 27.27% cases. In studies done by Sanguinetti et al. (2016) [10], 67% (31/47) were ER/ PR positive. Chao li and Xujung li et al (2022), 96% (25/26) were Both ER+ and PR+ and in study done by Majdouline El Fouhi et al (2022) [11], 83% (15/26) were ER+/PR+. Patients who showed positivity of ER/PR in MBC (83%) had recieved hormonotherapy (tamoxifen). Tamoxifen has been shown to lead to increased survival rates in women with hormone-sensitive disease and today is generally considered the standard adjuvant treatment for male breast cancer hormone-dependent. Also, hormonal therapy has been proven to help in metastatic disease in females and males.
In conclusion, hence, concluding from the above discussion, Male breast carcinoma presents later in life (age>60years) and it presents in advance stage of carcinoma(T4). Most common histopathological subtype is infiltrating ductal carcinoma. Most of the patients are receptor positive (ER/PR). Therefore Concerted efforts including education of public and health professionals, in order to make earlier diagnosis and thereby improve prognosis. Efforts should be made to improve outcomes, an interprofessional team approach that consists of an oncologist, surgeon, radiation therapist, dietitian, and mental health counselor is recommended. Earlier diagnosis and wide use of adjuvant treatments (RT/HT/ CT) widely decreased local recurrences and increased survival rates in male breast cancer .
Acknowledgments
We acknowledge the help extended by the Department of General Surgery,Rajendra Institute of Medical Sciences Ranchi, India.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Funding statement
There was no source of funding for this research
References
- The Epidemiology of Male Breast Cancer Ferzoco RM , Ruddy KJ . Current Oncology Reports.2016;18(1). CrossRef
- Male breast cancer. Evolution of treatment and prognostic factors. Analysis of 489 cases Cutuli B, Le-Nir CCS , Serin D, Kirova Y, Gaci Z, Lemanski C, De Lafontan B, et al . Critical Reviews in Oncology/Hematology.2010;73(3). CrossRef
- The rising incidence of male breast cancer Speirs V, Shaaban AM . Breast Cancer Research and Treatment.2009;115(2). CrossRef
- Male Breast Cancer: Epidemiology and Risk Factors Abdelwahab Yousef AJ . Seminars in Oncology.2017;44(4). CrossRef
- A contemporary review of male breast cancer: current evidence and unanswered questions Leon-Ferre RA , Giridhar KV , Hieken TJ , Mutter RW , Couch FJ , Jimenez RE , Hawse JR , et al . Cancer Metastasis Reviews.2018;37(4). CrossRef
- Male Breast Cancer: An Updated Surveillance, Epidemiology, and End Results Data Analysis Liu N, Johnson KJ , Ma CX . Clinical Breast Cancer.2018;18(5). CrossRef
- Synchronous bilateral breast cancer in men: a case report and review of the literature Sosnovskikh I, Naninato P, Gatti G, Caldarella P, Masullo M, De Brito LL , Luini A. Tumori.2007;93(2). CrossRef
- Male Breast Cancer—an Indian Multicenter Series of 106 Cases Chhabra MK , Chintamani C, Kadyaprath G, Srivastva A, Selvakumar VPP , Ranjan P, Durga C, et al . Indian Journal of Surgery.2019;83. CrossRef
- Case Series Analysis of Male Breast Cancer Li C, Li X. Indian Journal of Surgery.2022. CrossRef
- Sanguinetti A, et al . International Journal of Surgery Case Reports.2016;205:8-11.
- Male breast cancer: a report of 25 cases Fouhi ME , Mesfioui A, Benider A. The Pan African Medical Journal.2020;37. CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times