Dosimetric Comparison of Intensity-Modulated Radiation Therapy (IMRT) and Volumetric-Modulated Arc Therapy (VMAT) for Synchronous Bilateral Breast Cancer Irradiation: A Planning Study
Download
Abstract
Background and objective: The large radiation field and surrounding normal structures in synchronous bilateral breast cancer (SBBC) make treatment planning and dose delivery significantly more challenging than in unilateral breast cancer. Intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT) have the potential to improve target dose coverage while minimizing normal tissue exposure compared to 3D-conformal radiotherapy (3D-CRT). This study aimed to investigate the dosimetric variations of IMRT and VMAT techniques using a single isocenter for planning SBBC cases.
Material and methods: Five patients who had undergone bilateral mastectomy were included in this study. A dose of 50 Gy in 25 fractions was prescribed. VMAT and IMRT plans were created for each patient using a mono-isocentric approach. Dosimetric data for the target volume (PTV) and organs at risk (OARs) were compared.
Results: VMAT plans demonstrated a trend towards better PTV coverage compared to IMRT (V95 IMRT = 94.8720, V95 VMAT = 95.8740; P = 0.316). VMAT plans significantly improved dose homogeneity, with a decrease in V105% from 2.886% to 0.312% (P = 0.001). IMRT plans showed a trend towards higher lung mean dose (Dmean) and V20Gy compared to VMAT plans. The irradiation dose to the heart was significantly higher in the IMRT plans compared to VMAT plans, resulting in a higher Dmean (15.836 Gy vs 13.580 Gy; P = 0.026), V25Gy (16.498% vs 13.832%; P = 0.046), and V30Gy (9.774% vs 7.022%; P = 0.043).
Conclusion: The single-isocentric VMAT technique is a convenient approach for SBBC planning, improving target volume coverage with optimal normal tissue sparing. It is a feasible option for synchronous bilateral breast irradiation.
Introduction
Synchronous bilateral breast cancers are defined as two tumors diagnosed within an interval of 6 months. Synchronous bilateral breast cancer (SBBC) accounts for 2.1% of all breast cancers but the numbers of SBBC diagnoses have been showing an upward trend with an increase in the number of breast cancer cases [1]. Despite having a low incidence, SBBC has a much worse overall survival rate than unilateral breast cancer [2-3]. For the management of SBBC, there is no set standard.
The large radiation field, complex anatomy, and surrounding normal structures make treatment planning and dose delivery of SBBC much more difficult and time-consuming than it is for unilateral breast cancer radiotherapy. Using a tangential field configuration is one of the common treatment methods for SBBC [4-5]. The usual tangential field design either results in extensive beam overlap or under-doses some part of PTV. Inadequate coverage of the target structure or inhomogeneous dose distribution with hotspots, particularly in obese patients, are other limitations of the standard tangential approach. Another drawback is the inability to lower the high dosage volumes to the ipsilateral heart and lung.
Intensity-modulated radiation therapy (IMRT), volumetric-modulated arc therapy (VMAT), or helical tomotherapy (HT) can produce acceptable cosmetic effects and cardiac sparing while improving target dose coverage compared to 3D-CRT. To address this issue, a number of dosimetric studies using IMRT, VMAT, and helical tomotherapy have been conducted, and the findings are encouraging [6-9]. With this context in mind, we carried out a study to examine the dosimetric variations of IMRT or VMAT techniques using a single isocenter and to determine the best solutions with heart and other normal tissue sparing for SBBC.
Materials and Methods
Five patients were considered for this study. Prior informed consent was taken of each patient. All the patients had undergone bilateral mastectomy.
Patient details
Patient 1 was staged as pT2N2M0 in right breast and pT2N1M0 in left breast. She received radiotherapy to bilateral chest wall and lymph nodal region. Patient 2 was staged as pT2N3M0 in right breast and pT2N1M0 in left breast. She received radiotherapy to bilateral chest wall and lymph nodal region. Patient 3 was staged as pT2N0M0 in right breast and pT2N1M0 in left breast. Patient was taken for post operative radiotherapy to bilateral chest wall and lymph nodal region in left side only. Patient 4 was staged as pT3N0M0 in right breast and pT1N2M0 in left breast. She received adjuvant radiotherapy to bilateral chest wall and lymph node region in left side only. Patient 5 was staged as pT2N1M0 in right breast and pT4bN0M0 in left breast. She received radiotherapy to bilateral chest wall and lymph node region.
Dose prescribed was 50 Gy in 25 fractions in all the patients.
Target and OAR delineation
The RTOG (Radiation Therapy Oncology Group) atlas was used to contour the clinical target volume (CTV) for the breast and regional node [10].
CTV-chest wall was used to refer to the total volume of the chest wall. CTV-LN was used to describe the lymph node region, which included the supraclavicular and axillary levels I, II, and III. Planning target volumes (PTVs) were expanded 5 mm in all directions from CTV and pulled from the skin with a 3-mm skin gap from the surface. PTV was prescribed a total dose of 50 Gy given in 25 fractions with daily dose of 2 Gy per fraction. Ninety five percent of the specified dose was intended to cover 95 percent of PTV.
The entire heart and lungs were considered as organs at risk (OARs). The OAR constraints are mentioned in Table 1.
| OAR’S | Dose Recommendation |
| Mean lung dose | <15 Gy |
| Lungs | V20Gy <35% |
| Heart | V25Gy <20% |
As there is no definite treatment protocol for SBBC, the OAR dose constraints were established based on the results of previous SBBC studies and an attempt to maximize OAR sparing [11].
Treatment planning
Planning CT was performed with the patients immobilised in a supine position on a breast board with both arms lifted. The VMAT plans were generated on Monaco® treatment planning system (TPS) (version 5.11.03, Elekta AB) for Elekta Synergy linear accelerator with MLCi2 with 80 leaves. VMAT and IMRT plans were created for each patient. All the plans made were mono-isocentric.
VMAT plans
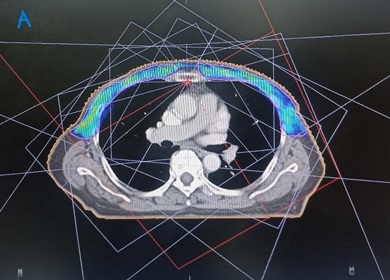
The plans were optimised simultaneously for all arcs with a single isocenter located below sternum (Figure 1).
Figure 1. Beam Arrangements, Isocentre Position and PTV Coverage with 95% Isodose in IMRT Plan.
Total 4 arcs (2 clockwise and 2 anti-clockwise) were used in planning with gantry angle of 195°–165°. The collimator angle of 30° was used for clockwise plans and 330° for anti-clockwise plans. Treatment plans were optimised with a maximum number of control points of 300 per arc, a minimum segment width of 1.0 cm and with high fluence smoothing. An autoflash margin of 1.5 cm and surface margin of 0.5 cm were used in the optimisation. A standard deviation of 1% was used in Monte Carlo (MC) dose calculation with a dose grid of 3.0 mm.
IMRT plans
For IMRT planning, 9-11 beams were used. The field arrangements are shown in Figure 2.
Figure 2. Beam Arrangements, Isocentre position and PTV Coverage with 95% Isodose in VMAT Plan.

Dynamic MLC (multi leaf collimator) with fixed gantry angles was utilised in IMRT plans. Plans were mono-isocentric with single isocenter located below sternum (Figure 2). Each field was spaced by 30–40 degrees. All beams were coplanar beams.
Treatment delivery
Image guidance with daily cone-beam CT (CBCT) was performed to verify treatment setup.
Plan analysis
Dosimetric data of the target and of OARs and dose-volume histograms (DVH), were compared.
Conformity of the plans was assessed by calculating conformity index (CI) through formula as follows:
CI = TVPIV2/(TV*PIV).
Here, TVPIV is the volume of target volume covered by prescription isodose, TV is target volume and PIV is prescription isodose volume.
The CI ranges from 0 to 1. A value of CI close to 1 reflects an improved PTV conformity.
According to ICRU report No.83, the HI was calculated as follows:
HI = (D2% − D98%)/D50%
Statistical analysis
The data was entered into a Microsoft Excel spreadsheet and analyzed using IBM SPSS Statistics for Windows, version 24 (IBM Corp., Armonk, NY, USA). A student’s paired t-test was performed to interpret the results, and a p-value of less than 0.05 was considered statistically significant.
Results
A total of 10 plans were made: one IMRT and one VMAT plan for each patient. All the plans were mono-isocentric. Table 2 and 3 summarizes the dosimetric comparison of the target and OAR doses of the plans respectively.
| PTV Parameters | IMRT | VMAT | P value |
| V95 (%) | 94.872±2.674 | 95.874±2.077 | 0.316 |
| V105 (%) | 2.886±0.507 | 0.3120±0.155 | 0.163 |
| V110 (%) | 0.00±0.000 | 0.00±0.000 | 0.001 |
| D98 (Gy) | 46.234±1.693 | 46.842±1.615 | 0.117 |
| D2 (Gy) | 51.922±0.167 | 52.716±0.085 | 0.001 |
| D mean (Gy) | 49.652±0.963 | 50.262±0.165 | 0.28 |
| D max (Gy) | 54.406±0.365 | 55.218±0.466 | 0.06 |
| CI | 0.734±0.033 | 0.755±0.046 | 0.403 |
| HI | 0.1206±0.029 | 0.1209±0.024 | 0.975 |
| MU | 1151.492±79.038 | 1003.118±87.537 | 0.034 |
Abbreviations, PTV- Planning target volume, V95- Volume of PTV receiving 95% of the prescription dose, V105- Volume of PTV receiving 105% of the prescription dose, V110- Volume of PTV receiving 110% of the prescription dose, D98- Dose received by 98% of the target volume, D2- Dose received by 2% of the target volume, D mean- Mean dose, D max-Maximum dose, CI- Conformity index, HI- Homogeneity index, MU- Monitor Units
| OAR Parameters | IMRT | VMAT | P value |
| Right lung | |||
| D mean | 18.464±1.599 | 17.582±1.160 | 0.325 |
| V5Gy (%) | 88.492±7.815 | 93.446±3.704 | 0.229 |
| V20Gy (%) | 35.280±3.820 | 32.448±2.604 | 0.171 |
| Left lung | |||
| D mean | 17.778±1.441 | 17.326±0.261 | 0.527 |
| V5Gy (%) | 85.922±7.335 | 89.404±4.254 | 0.096 |
| V20Gy (%) | 35.114±3.865 | 32.238±1.587 | 0.226 |
| Heart | |||
| D mean | 15.836±1.282 | 13.580±1.468 | 0.026 |
| V25Gy (%) | 16.498±2.874 | 13.832±3.678 | 0.046 |
| V30Gy (%) | 9.774±2.411 | 7.022±3.278 | 0.043 |
Abbreviations, OAR- Organ at risk, D mean- Mean dose, V5Gy- Volume of PTV receiving dose of 5 Gy, V20Gy- Volume of PTV receiving dose of 20 Gy, V25Gy- Volume of PTV receiving dose of 25 Gy, V30Gy- Volume of PTV receiving dose of 30 Gy
PTV coverage
The data for the dose distribution to the PTV of the IMRT and VMAT plans are summarized in Table 2. The PTV dose coverage was better using VMAT technique when compared to IMRT technique but the difference was not statistically significant (V95 IMRT=94.8720, V95 VMAT=95.8740; P=0.316). When compared to a IMRT technique, the VMAT plans significantly improved the dose homogeneity as the average V105% (V52.5Gy) decreased from 2.886% to 0.312% using VMAT plans (P=0.001). There was no significant difference in D2%, CI and HI values. D98% showed significant differences between IMRT and VMAT plans with mean values of 46.234 Gy and 46.842 Gy respectively (P=0.001).
Table 2 also hows the average MU per fraction for the different plans, and the difference in MUs was significant with VMAT plans having lesser number of MU segments than IMRT plans (1151.492 vs 1003.118; P=0.034).
Abbreviations, PTV- Planning target volume, V95- Volume of PTV receiving 95% of the prescription dose, V105- Volume of PTV receiving 105% of the prescription dose, V110- Volume of PTV receiving 110% of the prescription dose, D98- Dose received by 98% of the target volume, D2- Dose received by 2% of the target volume, D mean- Mean dose, D max-Maximum dose, CI- Conformity index, HI- Homogeneity index, MU- Monitor Units
As VMAT plans obtained the lesser number of MUs, the delivery time was notably reduced.
OAR dose
Table 3 shows the statistical comparison of the OAR dose distribution for IMRT and VMAT plans. Regarding the lung doses, IMRT plans showed trend towards higher Dmean and V20Gy than VMAT plans although the difference was not statistically significant. The average Dmean of right lung was 18.464 and 17.582 in IMRT and VMAT plans respectively (P=0.325) while the average Dmean of left lung was 17.778 and 17.326 in IMRT and VMAT plans respectively. V5Gy of right lung was 88.492 and 93.446 in IMRT and VMAT respectively (P=0.229) while V5Gy of left lung was 85.922 and 89.404 in IMRT and VMAT plans respectively (P=0.096). V20Gy of right lung was 35.28 and 32.448 in IMRT and VMAT respectively (P=0.171) while V20Gy of left lung was 35.114 and 32.238 in IMRT and VMAT plans respectively (P=0.226).
The irradiation dose to the heart was significantly higher in the IMRT plan than VMAT plan, resulting in Dmean of 15.836 Gy vs 13.580 Gy (P=0.026), volume of the heart receiving doses greater than 25 Gy (V25Gy) of 16.498% vs 13.832% (P=0.046) and V30 Gy of 9.774% vs 7.022% (P= 0.043).
Overall, the VMAT treatment plans decreased the doses to the lungs and heart. The main drawback considering the VMAT planning was a slight increase in the low dose volume (V5Gy).
Discussion
The planning approach for synchronous BBC radiation using a single isocentre VMAT and IMRT technique is described in this study. This study looked into the best radiotherapy planning strategy for SBBC, particularly when regional LN irradiation was included. For treating the bilateral breasts and the local LN area, the PTV is quite large. Therefore, compared to the PTV of unilateral breast cancer, radiation exposure to OARs, such as the heart and lungs increases. It is difficult to treat SBBC with tangential field configurations because, in most circumstances, field overlapping cannot be prevented. The primary benefit of these techniques is the avoidance of the significant field overlapping issues associated with tangential field designs. Therefore, overlapping areas with significant hotspots should be avoided to prevent skin damage. Additionally, to reduce the likelihood of a tumour recurrence, the PTV area should receive the prescribed dose without cold spots. As we know, SBBC involves a large target volume and is closer to OARs, such as the heart and lungs. The incidence of acute and late toxicities, such as acute radiodermatitis, symptomatic radiation pneumonitis, and skin fibrosis, is reduced with the reduction of the high dose region. It has been demonstrated that the VMAT technique reduces the amount of tissue that is exposed to high radiation doses. But there is a concern that by increasing the amount of tissue exposed to low doses of radiation, VMAT technique can increase the risk of radiation-induced carcinogenesis.
In a study by Kim et al., with 3D‐CRT for SBBC V95% was 93.65 ± 2.81% for the left side PTV and 93.48 ± 2.74% for the right side PTV [11]. In this study, in terms of target and OAR dose distribution, IMRT was found to be superior than VMAT and 3D-CRT. 3D-CRT was advantageous in terms of OAR low dose distribution. In a study by Nicolini et al, VMAT showed dosimetric improvements with respect to IMRT [7]. High sparing of lungs was achieved with both techniques. The observed differences on mean lung dose were not statistically significant. At medium to high levels, VMAT proved to be slightly superior to IMRT. At low dose levels, e.g. V5 Gy, IMRT was better than VMAT. Delivery parameters confirmed its logistical advantages and pre-treatment dosimetry proved its reliability. Similarly, in our study the PTV dose coverage was better using VMAT technique when compared to IMRT technique but the difference was not statistically significant (V95 IMRT=94.8720, V95 VMAT=95.8740; P=0.316). Regarding the lung doses, IMRT plans showed trend towards higher Dmean and V20Gy than VMAT plans although the difference was not statistically significant. The irradiation dose to the heart was significantly higher in the IMRT plan than VMAT plan.
Most dosimetric studies on SBBC irradiation, such as IMRT, VMAT, or helical tomotherapy, used a single isocenter beneath the sternum [6-8]. This method can offer a more simpler plan that is easier to deliver, but its clinical use may be restricted, especially in case of obese individuals and patients with bigger target volume. Dual-isocentric plans requires two image-guidance captures per fraction in each application. They not only take longer time to implement but also require more careful work compared to mono-isocentric plans in terms of planning [12]. In a study by Nicolini et al., plans were optimised with two arcs of 360° each. The first arc, rotating clockwise, was incident primarily on the right breast, the second arc, rotating counter-clockwise, was incident on the left breast. The same isocentre (beneath the sternum) was used for IMRT and VMAT planning techniques [7]. In a study by Seppala et al, a single isocentre VMAT technique was implemented for BBI. With the VMAT techniques, the dose delivery was quick and the hotspots in the field over-lapping areas were avoided. The PTV dose coverage was superior in VMAT plans when compared with conventional tangential technique plans [8]. In a study by Huang et al., better hot spot control was seen with single isocentric fixed-jaw IMRT treatment technique than other treatment modalities. A mono-isocentric approach for IMRT planning was used in this study [13]. In the present study, we used single isocentre for both IMRT and VMAT planning thus making treatment delivery simpler. The 2018 ASTRO Guideline recommends that for hypofractionated whole-breast irradiation (HFWBI), regardless of dose fractionation, the volume of breast tissue receiving 105 percent of the prescribed dose should be kept to a minimum [14]. In our study, when compared to a IMRT technique, the VMAT plans significantly improved the dose homogeneity as the average V105% (V52.5Gy) decreased from 2.886% to 0.312% using VMAT plans (P=0.001).
We need to concentrate on more sophisticated planning strategies in situations where SBBC requires irradiation. Our study provides an alternative RT planning strategy for SBBC irradiation with highly conformal RT techniques while assuring adequate normal tissue sparing. Our study emphasises the potential of VMAT and IMRT approaches to improve the dose distributions in the treated region while sparing normal tissue and reducing patient toxicity. The treatment procedure is also made simpler by using a single isocenter, which cuts down on the time spent on the treatment device.
Our study has some limitations. Firstly, the study was carried out in a single centre with a small sample size, too imprecise to draw a definite conclusion. Hence, a multi-centre investigation with a larger sample size and longer follow-up duration is required to find an accurate comparison. Secondly, in this study only the dosimetric parameters of IMRT and VMAT plans were evaluated. We did not study the correlation of the dosimetric parameters with toxicity profile in patients of SBBC. Future studies should be carried out to study the clinical significance of the same. Lastly, we had all post mastectomy patients in our study.
In conclusion, this study illustrates the feasibility of using the VMAT approach to treat bilateral breast cancer. The single isocentric VMAT technique can be performed conveniently with a decreased setup time. It improves target volume dose homogeneity, normal tissue sparing and prevents field overlapping issues. Additional research on the ideal RT planning techniques should be conducted with a bigger participant pool in order to strike a balance between dosimetric and therapeutic efficacy.
Funding and Conflict of Interest
None
References
- Synchronous, bilateral breast cancer: prognostic value and incidence Jobsen JJ , Palen J, Ong F, Meerwaldt JH . Breast (Edinburgh, Scotland).2003;12(2). CrossRef
- Bilateral breast cancer, synchronous and metachronous; differences and outcome Jobsen JJ , Palen J, Ong F, Riemersma S, Struikmans H. Breast Cancer Research and Treatment.2015;153(2). CrossRef
- Bilateral breast cancer: analysis of incidence, outcome, survival and disease characteristics Kheirelseid EAH , Jumustafa H, Miller N, Curran C, Sweeney K, Malone C, McLaughlin R, Newell J, Kerin MJ . Breast Cancer Research and Treatment.2011;126(1). CrossRef
- Bilateral breast-conserving therapy for bilateral breast cancer: results and consideration of radiation technique Yamauchi C, Mitsumori M, Nagata Y, Kokubo M, Inamoto T, Mise K, Kodama H, Hiraoka M. Breast Cancer (Tokyo, Japan).2005;12(2). CrossRef
- Early-stage bilateral breast cancer treated with breast-conserving surgery and definitive irradiation: the University of Pennsylvania experience Fung MC , Schultz DJ , Solin LJ . International Journal of Radiation Oncology, Biology, Physics.1997;38(5). CrossRef
- Bilateral breast and regional nodal irradiation in early stage breast cancer‑a dosimetric comparison of IMRT and 3D conformal radiation therapy Yusoff S, Chia D, Tang J, Lu J. Int J Radiat Oncol Biol Phys.2012;84:S223.
- Simultaneous integrated boost radiotherapy for bilateral breast: a treatment planning and dosimetric comparison for volumetric modulated arc and fixed field intensity modulated therapy Nicolini G, Clivio A, Fogliata A, Vanetti E, Cozzi L. Radiation Oncology (London, England).2009;4. CrossRef
- Volumetric modulated arc therapy for synchronous bilateral whole breast irradiation - A case study Seppälä J, Heikkilä J, Myllyoja K, Koskela K. Reports of Practical Oncology and Radiotherapy: Journal of Greatpoland Cancer Center in Poznan and Polish Society of Radiation Oncology.2015;20(5). CrossRef
- Helical tomotherapy in patients with breast cancer and complex treatment volumes Cendales R, Schiappacasse L, Schnitman F, García G, Marsiglia H. Clinical & Translational Oncology: Official Publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico.2011;13(4). CrossRef
- Delineation of target volumes and organs at risk in adjuvant radiotherapy of early breast cancer: national guidelines and contouring atlas by the Danish Breast Cancer Cooperative Group Nielsen MH , Berg M, Pedersen AN , Andersen K, Glavicic V, Jakobsen EH , Jensen I, et al . Acta Oncologica (Stockholm, Sweden).2013;52(4). CrossRef
- Radiation therapy of synchronous bilateral breast carcinoma (SBBC) using multiple techniques Kim SJ , Lee MJ , Youn SM . Medical Dosimetry: Official Journal of the American Association of Medical Dosimetrists.2018;43(1). CrossRef
- Dual‑isocentric volumetric modulated arc therapy in synchronous bilateral breast cancer irradiation: A dosimetric study Rakici SY , Cinar Y. J Radiat Cancer Res.2020;11:188-193.
- Evaluation of fixed-jaw IMRT and tangential partial-VMAT radiotherapy plans for synchronous bilateral breast cancer irradiation based on a dosimetric study Huang J, Wu X, Lin X, Shi J, Ma Y, Duan S, Huang X. Journal of Applied Clinical Medical Physics.2019;20(9). CrossRef
- Radiation therapy for the whole breast: Executive summary of an American Society for Radiation Oncology (ASTRO) evidence-based guideline Smith BD , Bellon JR , Blitzblau R, Freedman G, Haffty B, Hahn C, Halberg F, et al . Practical Radiation Oncology.2018;8(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times