Perinephric and Ovarian Metastasis from Advanced Urothelial Carcinoma of the Bladder: A Rare Dismal Disease - A Case Report
Download
Abstract
Background: Metastatic urothelial carcinoma of the bladder is a rarely encountered condition at the time of diagnosis, with lymph nodes, bones, lungs, and liver being the common sites of metastasis. However, metastasis can also occur in uncommon locations.
Case Presentation: This case report describes the unusual occurrence of metastasis in the perinephric region, renal fascia, and ovaries. It highlights the importance of distinguishing primary urothelial carcinoma of the ovary from metastatic lesions. Due to the lack of standardized treatment guidelines, management options should be tailored to each individual case. The prognosis of metastatic urothelial carcinoma remains unfavorable, with a limited life expectancy.
Conclusion: This case report presents a case of metastatic urothelial carcinoma of the bladder with perinephric region and ovarian metastasis, detailing the course of treatment.
Introduction
Ninety percent of bladder tumours are Urothelial or Transitional cell carcinomas (TCC) and rest of them are other rare histological variants [1]. Metastasis accounts for only 5% of cases at diagnosis with poor prognosis of 5-year overall survival being less than 5%. Lymph nodes, bones, lung, liver, and peritoneum are the most common sites of metastasis from bladder cancer [2]. Perinephric space is an unusual site for metastasis and the metastasis are seen as multiple discrete soft tissue nodules. Due to lymphatic connections between perinephric space and mediastinum, primary from lungs are the most common site for metastasis in this space [3]. Rest of the malignancies spread through haematogenous route and are seen commonly from melanoma, prostate, breast and gastrointestinal tumours [4]. Metastasis from adjacent solid organs can also take place in the perinephric space, which should be assessed for the same [5]. Metastasis in perinephric space from urinary bladder carcinoma is very rare presentation in literature and till date there is no case reported with the same as per our knowledge. Here, we present a case of urothelial carcinoma bladder with upfront metastasis in perinephric space, ovaries, ureter, mesentry and lymph nodes with dilemma in diagnosis and management of this patient.
Case Report
Sixty years old hypertensive female presented in gynaecology department with irregular bleeding per vaginum and haematuria on and off for last one year. On examination, growth was felt over the cervix and anterior wall of vagina which bleeds on touch. With suspicion of carcinoma cervix, patient underwent cervical biopsy which was suggestive of moderately differentiated squamous cell carcinoma. Upon investigating the patient, the kidney function tests were found to be deranged (Urea- 83 mg/dL, creatinine – 5.48 mg/dL) with normocytic normochromic anaemia. On ultrasonography, mild bilateral hydronephrosis with left perinephric collection was seen with irregular thickening in left lateral and posterior urinary bladder wall involving left vesicoureteric junction (VUJ). Per cutaneous nephrostomy was done and then she underwent contrast enhanced computed tomography abdomen and pelvis which was suggestive of asymmetrical irregular thickening of posterior and left lateral wall of urinary bladder measuring upto 15 mm with infiltration of bilateral vesicoureteric junction and bilateral distal ureter with mild hydrouretronephrosis (HDUN) (Figure 1).
Figure 1. a-b, Axial CECT Abdomen Images Showing Posterolateral Urinary Bladder Wall Thickening Infiltrating Bilateral VUJ. c-e, Necrotic inguinal, bilateral external iliac, pre and paraaortic lymph nodes. f, Right ovarian and pelvic necrotic deposits with poor fat planes with sigmoid colon and ileum. g-h, Bilateral hydrouretronephrosis with left perinephric fascial thickening, soft tissue deposits along fascia and perinephric fluid collection. k-o, Coronal CECT images showing left perinephric fluid collection and soft tissue deposits in perinephric space. 1p, Saggital CECT, showing growth along posterior wall of urinary bladder infiltrating into cervix.
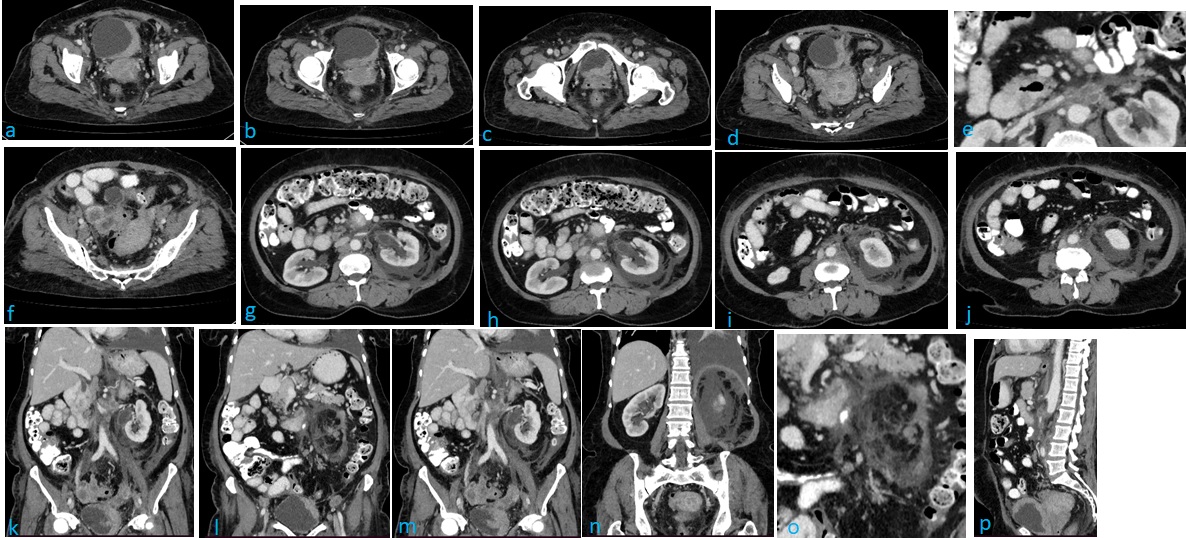
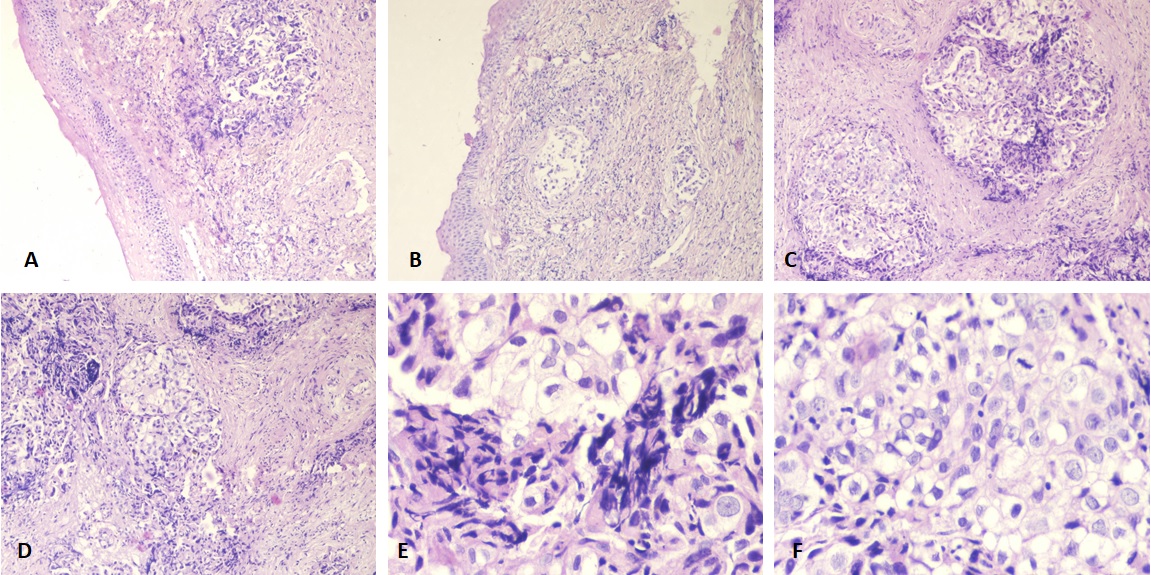
This growth was infiltrating into perivesical fat, anterior wall of vagina and cervix. Numerous heterogeneously enhancing centrally necrotic enlarged lymph nodes are seen at bilateral inguinal, bilateral external, internal iliac, common iliac and retroperitoneal region largest measuring 2cm in short axis diameter (SAD). Multiple heterogeneously enhancing centrally necrotic metastatic deposits are seen in pelvis, right ovary (3.7x2.6cm), mesenteric (2.2x1.9cm) with loss of fat planes with adjacent sigmoid colon and ileal loops. Left kidney shows enhancing thickening of dilated pelvicalyceal system and upper ureter with multiple variable sized heterogeneously enhancing perinephric deposits, moderate perinephric free fluid, stranding and nodular enhancing thickening of left anterior, posterior and lateroconal fascia. The value of CA-125 was 180 units/ml. With these findings the pathology slides were reviewed, which showed transitional cell carcinoma (Figure 2) and the patient was started on palliative chemotherapy based on Injection Gemcitabine and Injection Cisplatin for urothelial carcinoma bladder.
Figure 2. A-D, Cervical Biopsy Tissue Lined by Stratified Squamous Epithelium. Subepithelial stroma shows infiltration by the nest of tumour cells. (Hematoxylin and Eosin, 100x). E and F, Show cervical stromal infiltration by tumour nests revealing polyhedral tumour cells with nuclear atypia. (Hematoxylin and Eosin, 200x).
After three cycles of chemotherapy, PET-CT (Positron Emission Tomography-Computed Tomography) scan was done which showed mildly FDG avid (SUVmax 3.4) thickening (15 mm) of left lateral and posterolateral wall of urinary bladder with hypermetabolic cervical, supraclavicular, axillary, portocaval, peripancreatic, lateral paraaortic (SUVmax 4, size 1.7x1.3cm), left common iliac, bilateral external iliac and inguinal lymph nodes (Figure 3).
Figure 3.Post Three Cycles of Chemotherapy Imaging Study Showing (a) FDG avid left cervical lymph node, (b) left axillary nodes, (c) resolution of perinephric fluid collection and fascial thickening, (d) reduced soft tissue deposits along renal fascia, (e) reduced bilateral external iliac lymph nodes, (f) reduced bladder wall thickness.
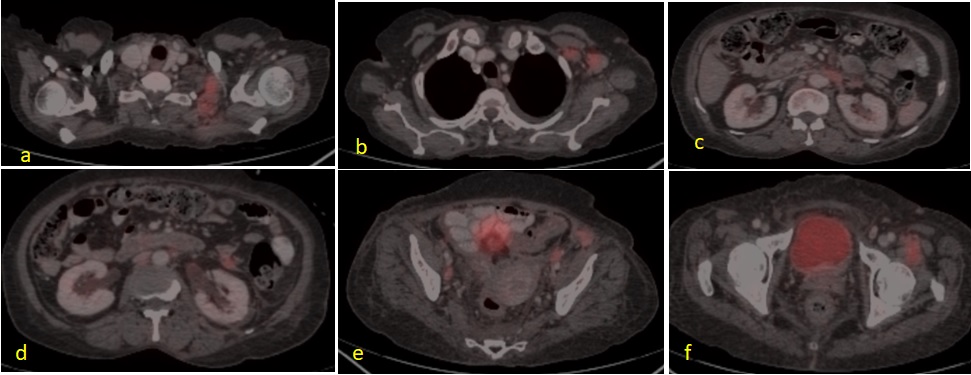
FDG avid (SUV max 4.4) ill defined left renal hilar lymph nodes were also seen. But the thickening and nodules seen in perinephric region had regressed. Also soft tissue deposits in ovary and mesentry were not seen after three cycles of chemotherapy. The patient is planned for three more cycles of chemotherapy.
Discussion
Metastatic bladder carcinoma is seen in 5% of patients [2]. The most common sites of metastasis are pelvic lymph nodes followed by bone, lung, liver and peritoneum [2]. Many atypical sites of metastasis from bladder carcinoma have been reported till date. These include heart, kidney, spleen, pancreas, brain, ovary, prostate and testis in 1 to 8% of the patients [6]. A few case reports have also demonstrated deposits to sites including nephrostomy tracts, laparoscopic and abdominal incisions, labia minora and umbilicus [7]. Metastasis from a case of urothelial carcinoma bladder to perinephric space and ovaries is an unusual finding. There are a very few reports of primary urothelial carcinoma metastasizing to ovary and negligible data on perinephric metastasis.
Retroperitoneum is divided into three compartments: perinephric space, anterior and posterior pararenal space [8]. Perinephric region is bordered by pararenal spaces anteriorly and posteriorly and is inverted cone in shape corresponding to embryological development of renal system from pelvis [4] (Figure 4).
Figure 4. CECT Abdomen Showing Inverted Cone Shaped Perinephric Space (red arrow), Bounded by Anterior Renal Fascia (yellow arrow) and posterior renal fascia (green arrow) in axial (a) and saggital (b) sections with thickened lateral conal fascia (blue arrow).
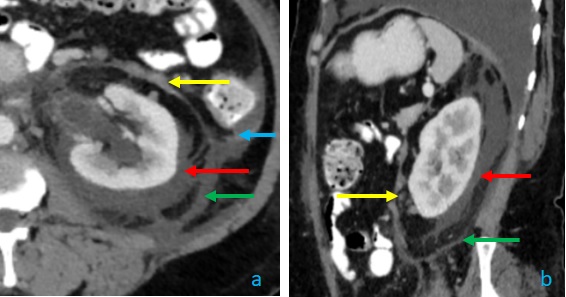
This space contains kidneys, adrenal glands, proximal ureters, fat, bridging septa, vessels and lymphatics.
Due to the central location of this space in retroperitoneum disease manifestation and transmission can be seen rapidly.
Metastasis are seen in the form of nodules, masses or diffuse renal fat infiltration or stranding [9]. Stranding and nodular thickening of renal fascia as a metastatic feature is uncommon as seen in the above-mentioned patient. The differential diagnosis of these metastasis can be fatty tissue infection, retroperitoneal haemorrhage, perirenal lymphoma and liposarcoma [10]. Pulmonary malignancies have predilection for metastasis in perinephric space due to lymphatic connections between perirenal space and mediastinum. Metastasis from prostate, breast, gastrointestinal tract and melanomas in perinephric space can be seen through haematogenous spread [3].
It is very rare to have isolated perirenal metastasis and these are usually seen with metastasis at multiple other sites too. In our case, multiple metastatic deposits were seen in pelvis, ovary, mesentry, lymphnodes and renal fascia with perinephric space.
Metastatic urothelial carcinoma in ovaries from bladder or urinary system is extremely rare with only a few cases reported in the literature. In all of those cases, the metastasis were seen in unilateral ovary which were synchronous as well as metachronous [11]. Primary ovarian transitional cell carcinoma needs to be kept as a differential as it has modest response to chemotherapy whereas metastatic urothelial carcinoma bladder is fatal. To date, on the basis of limited evidence, there is no consensus on how to optimally approach such patients. Multidisciplinary approach is required and the treatment for each case should be individualised.
In conclusion, to our knowledge, this is the first case report of urothelial carcinoma bladder metastasizing to perinephric space, renal fascia and ovary synchronously, causing challenge in primary diagnosis and management.
List of abbreviations
TCC, Transitional cell carcinoma; VUJ, Vesico Ureteric Junction; HDUN, hydrouretronephrosis; SAD, Short Axis Diameter; PET-CT, Positron Emission Tomography-Computed; Tomography; CA-125, Cancer
Antigen125; FDG, Fluorodeoxyglucose; SUV max, Maximum Standardized Uptake Value; CECT, Contrast Enhanced Computed Tomography
References
- Epidemiology of Bladder Cancer Saginala K, Barsouk A, Aluru JS , Rawla P, Padala SA , Barsouk A. Medical Sciences (Basel, Switzerland).2020;8(1). CrossRef
- Metastatic pattern of bladder cancer: correlation with the characteristics of the primary tumor Shinagare AB , Ramaiya NH , Jagannathan JP , Fennessy FM , Taplin M, Van den Abbeele AD . AJR. American journal of roentgenology.2011;196(1). CrossRef
- Perirenal metastases from lung cancer: CT diagnosis Wilbur AC , Turk JN , Capek V. Journal of Computer Assisted Tomography.1992;16(4). CrossRef
- Radiological diagnosis of perinephric pathology: pictorial essay 2015 Mitreski G, Sutherland T. Insights into Imaging.2017;8(1). CrossRef
- Neoplastic and proliferative disorders of the perinephric space Heller MT , Haarer KA , Thomas E, Thaete FL . Clinical Radiology.2012;67(11). CrossRef
- Metastatic transitional cell carcinoma of the urinary bladder to the shoulder girdle Weizer AZ , Shariat SF , Haddad JL , Escudier S, Lerner SP . Reviews in Urology.2002;4(2).
- Metastases from transitional cell carcinoma of urinary bladder Babaian RJ , Johnson DE , Llamas L, Ayala AG . Urology.1980;16(2). CrossRef
- Peritoneal and retroperitoneal anatomy and its relevance for cross-sectional imaging Tirkes T, Sandrasegaran K, Patel AA , Hollar MA , Tejada JG , Tann M, Akisik FM , Lappas JC . Radiographics: A Review Publication of the Radiological Society of North America, Inc.2012;32(2). CrossRef
- Unusual presentation of perirenal lung metastases D'Souza DL , Heinze SB , Dowling RJ . Australasian Radiology.2006;50(3). CrossRef
- Unusual Perirenal Metastasis from Lung Adenocarcinoma Basara I, Altay C, Seçil M. J Urol Surg.2015;2:169-170.
- Metastasis to the ovaries from transitional cell carcinoma of the bladder and renal pelvis: a report of two cases Lee M, Jung YW , Kim SW , Kim SH , Kim YT . Journal of Gynecologic Oncology.2010;21(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times