Primary Extranodal Lymphoma – A Three Year Study in a Tertiary Care Centre
Download
Abstract
Introduction: Primary extranodal lymphoma ( pENL ) is a group of lymphomas arising from tissues other than lymph nodes. Although the incidence of extranodal non Hodgkin lymphoma (ENL) is increasing worldwide, data is minimal.
Aims and objectives: To study the prevalence, anatomical distribution, clinical factors, and histological subtypes of extranodal lymphoma.
Materials and methods: This was a retrospective observational study conducted in the Department of Oncopathology in a regional cancer centre where we retrieved 103 cases of primary extranodal lymphoma ( pENL ) out of 380 cases of lymphoma from the institute’s data registry that were diagnosed over a period of three years from January 2017 to December 2019.
Result: There were 103 patients with primary extranodal lymphoma out of 380 patients with lymphoma, including 68 males and 35 females (M: F = 1.9:1), and the peak incidence occurred during the 4th to 5th decades of life. The age range was 4-80 years, and the mean age was 45.9 years. The median age was 50 years ± 19.2 years. The commonest site was the gastrointestinal tract (GIT) (31.8%), followed by the breast (15.5%). B-cell lymphoma was more common than T-cell lymphoma. The most frequent histopathological types of B-cell lymphoma were diffuse large B-cell lymphoma (DLBCL) (47%), Burkitt lymphoma (BL) (13%) and marginal zone lymphoma (MZL), (6%). Most of the patients in the pENL group were diagnosed to have Stage I/II lymphoma whereas Stage III/IV was more common in patients with nodal NHL. Most of the patients were treated with chemotherapy following the diagnosis. The most common chemotherapy used was cyclophosphamide, doxorubicin, vincristine, and prednisolone regimen, and rituximab was a part of chemotherapy.
Conclusion: Primary extranodal lymphomas constitute a diverse group of haematolymphoid malignancies. The diagnosis is a frequent challenge for pathologists, due to their morphological, characteristics and varied clinical presentations. Immunohistochemistry plays a major role in the diagnosis of primary extranodal lymphoma. Compared to the published series, no difference was noted regarding sex predilection or morphology. However, as this was mostly an epidemiological and morphological study, data about the detailed therapeutic outcomes are lacking.
Introduction
Primary extranodal lymphoma (pENL) is a group of lymphomas arising from tissues other than lymph nodes. Although the incidence of extranodal non Hodgkin lymphoma is increasing worldwide, data is minimal. Over the last decade, the International Extranodal Lymphoma Study Group (IELSG) has performed several retrospective and prospective trials to clarify the specific features of pENL [1]. In fact, great geographic variability in the overall frequency of extranodal presentations as well as the distribution of extranodal presentations across various anatomic sites of onset has been described [2]. For the definition, there is no consensus about the staging of primary extranodal lymphomas: the Ann Arbor staging system is currently widely used for describing the extent of the disease [1].
Aims and objectives
To study the prevalence, anatomical distribution, clinical factors, and histological subtypes of primary extranodal lymphoma.
Materials and Methods
Study design and site
This was a retrospective observational study conducted in the Department of Oncopathology in a regional cancer centre where we retrieved 103 cases of primary extranodal lymphoma (pENL ) out of 380 cases of lymphoma from the institute’s data registry that were diagnosed over a period of three years from January 2017 to December 2019.
Inclusion criteria: A primary extranodal lymphoma (PENL) was defined by presentation in extranodal organs (organs other than the lymph nodes).
Exclusion criteria: Patients with nodal lymphoma with extranodal involvement were excluded.
Data gathering
The demographic data, including age, sex, clinical signs and symptoms at presentation, stage of cancer, haemoglobin (Hb) level, platelet count, absolute lymphocyte count (ALC), biochemical parameters such as lactate dehydrogenase (LDH) and treatment modalities, were obtained from the medical records. Staging of lymphoma was done performed by clinical evaluation, computed tomography (CT) scans, and bone marrow aspiration and trephine biopsy as described in the standard recommendations and classified according to the modified Ann Arbor staging system.
Histopathology
The tissue was routinely processed in 10% formalin, and 5 μm paraffin sections were stained with hematoxylin and eosin. Immunohistochemistry (IHC) was performed using a panel of antibodies depending on the morphology.
The panel of antibodies used for IHC included pan-cytokeratin, leukocyte common antigen CD45, CD3, CD4, CD5, CD7, CD8, CD19, CD20, CD23, CD10,CD15, CD30, CD99, CD56, Bcl2, Bcl6, Tdt, anaplastic lymphoma kinase-1 (ALK-1), cyclinD1, Ki67 and epithelial membrane antigen (EMA), MUM 1, cMyc. A Ventana Benchmark Ultra machine automated staining system was used.
Peripheral blood, bone marrow aspiration and trephine biopsies
The bone marrow or peripheral blood was collected in an ethylenediaminetetraacetic acid (EDTA) vacutainer.Morphological evaluation was performed on Wright- stained peripheral smears and bone marrow aspirates.All the samples were processed within 24 hours. If the bone marrow aspiration and peripheral smear showed involvement by lymphoma, involvement by lymphoma on morphology was also subjected to IHC for confirmation.
Statistical analysis
Statistical analysis was performed using Microsoft Excel. The qualitative data are presented as frequencies and percentages, and the quantitative data are presented as the means or medians.
Results
There were 103 patients with primary extranodal lymphoma out of 380 patients with lymphoma, including 68 males and 35 females (M: F = 1.9:1), and the peak incidence occurred during the 4th to 5th decades of life.
The age range was 4-80 years, and the mean age was 45.9 years. The median age was 50 years ± 19.2 years. The detailed patient characteristics are listed in Table 1.
| Patient’s characteristics | Number | |
| Mean platelet volume (cells/mm3) | 3.6± 1.9 lakhs | |
| Mean Haemoglobin (g/dl ) | 10.58±2.060 | |
| Median LDH | 592.06 | |
| Immunocompromised status | 7/103 | |
| Bone marrow involvement | 8/103 | |
| Bulky disease | 13/103 | |
| Effusion | 2/103 | |
| Stage (N) | I | 37 |
| Ann Arbor stage | II | 44 |
| IV | 22 |
The commonest site was the gastrointestinal tract (GIT) (31.8%), followed by the breast (15.5%) (Table 2).
| Sites | No. of cases (percentage) |
| Gastrointestinal tract | 41 (39.8) |
| Stomach | 14 (13.59) |
| GE Junction | 1 (0.9) |
| Duodenum | 3 (2.9) |
| Jejunum | 3 (2.9) |
| Ileum | 7 (6.7) |
| Colon | 2 (1.9) |
| Caecum | 3 (2.9) |
| Liver | 3 (2.9) |
| Spleen | 1 (0.9) |
| Pancreas | 4 (3.8) |
| Head and neck | 7 (6.7) |
| Tongue | 2 (1.9) |
| Vallecula | 1 (0.9) |
| Nasopharynx | 1 (0.9) |
| Nostril | 1 (0.9) |
| Hard palate | 1 (0.9) |
| Thyroid | 1 (0.9) |
| Kidney | 1 (0.9) |
| Testis | 1 (0.9) |
| Ovary | 7 (6.7) |
| Breast | 16 (15.5) |
| Lung | 1 (0.9) |
| CNS | 4 (3.8) |
| Bone | 9 (8.73) |
| Skin and soft tissue | 10 (9.7) |
| Retroperitoneum | 3 (2.9) |
| Mediastinum | 2 (1.9) |
Among the primary gastrointestinal lymphomas, the most common site of involvement was the stomach in 14 cases (34.1%), followed by the ileum in 7 cases (6.7%).
There were 16 patients (15.5%) with breast lymphoma. Right sided breast involvement was greater than left sided breast involvement (56.2% vs 43.7%).
Cutaneous lymphoma comprised 10 (9.7%) patients. Details about the sites of primary extranodal lymphoma are provided in Table 3.
| Histopathological type | Frequency |
| Anaplastic Large cell lymphoma | 4 |
| B cell lymphoblastic lymphoma | 1 |
| Burkitt lymphoma | 13 |
| Diffuse large B cell lymphoma- GCB type | 30 |
| Diffuse large B cell lymphoma -ABC type | 20 |
| Extranodal NK/T Cell lymphoma Nasal type | 1 |
| Follicular lymphoma | 2 |
| Mantle cell lymphoma | 1 |
| Marginal zone lymphoma (Malt lymphoma) | 6 |
| Monomomorphic post Transplant lymphoproliferative lymphoma Peripheral T cell lymphoma NOS | 1 |
| High grade Non-Hodgkin B cell Lymphoma NOS | 12 |
| Plasmablastic lymphoma | 2 |
| Primary cutaneous peripheral T Cell lymphoma NOS | 4 |
| T Cell Lymphoblastic lymphoma | 3 |
| T cell rich large B cell lymphoma | 1 |
B-cell lymphoma was more common than T-cell lymphoma. The most frequent histopathological types of B-cell lymphoma were diffuse large B-cell lymphoma (DLBCL) (47%), Burkitt lymphoma (BL) (13%) and marginal zone lymphoma (MZL), (6%). Germinal centre (GC) or nongerminal centre (non-GC) phenotypic subtyping was based on immunohistochemistry using the Hans algorithm.
Among the T-cell lymphomas most common were primary cutaneous T-cell lymphoma (NOS) 4 (3.8%).
Bone marrow involvement was noted in 8/103 patients and was detected via both aspiration and biopsy. The most common cases were stage II with 47 cases (45.6%) followed by stage I 21 cases ( 20.38%) followed by stage IV with 22 cases (21.3%). Refer to Table 1.
There were 14 patients with pediatric extranodal lymphoma in our study. The most common site of presentation was the ileum. The most common histopathological type was Burkitt lymphoma.
Discussion
According to the literature, primary extranodal lymphoma (PENL) is a rare disease constituting approximately 20-24% of lymphomas. The frequency varies in different parts of the world. The findings of the present study were compared with previously available literature data.
The mean age in the present study was 45.9 years, which was similar to the findings of Vural F. et al. [3] (47 years) and K. S. Dhumure et al. [4] (46.7 years ). The male: female ratio was 1.9:1, which is similar to that reported by Wang GB et al [5].
Poorly differentiated or undifferentiated malignancies are always a challenge for pathologists in ascertaining lineage. This is a particularly difficult task when dealing with extranodal sites. Depending on the site and also the histological picture, we used a panel of markers. The differential diagnosis in most of the patients were poorly differentiated tumours and malignant round cell tumours, while in others, we could type it as NHL, but for subtyping, IHC was helpful.
In our study, 88.3% of the patients had B-cell lymphoma and 11.6% had T-cell lymphoma. GI tract involvement in NHL accounts for 30%–40% of cases of extranodal lymphoma. In our study, the GIT was the commonest site for primary extranodal lymphoma (41%), with the stomach being the most affected organ, which is consistent with the findings of Kroll A.D. G. et al [6]. Different histological subtypes of lymphoma can arise in the GIT. In our study, the most common type of GI lymphoma was DLBCL, which was 57% gastric and 21% intestinal in location.
Malt lymphoma represents approximately 35% of primary gastric lymphomas and less than 10% of intestinal lymphomas [1]. Colonization of lymphoid follicles by neoplastic infiltrates may be difficult to differentiate from cases of follicular lymphoma, especially in small and distorted biopsies. The distinction of neoplastic Malt from reactive Malt may be problematic in small biopsies from any extranodal site, and repeat biopsies may be necessary to achieve a diagnosis.
Burkitt’s lymphoma patients present with an abdominal mass, and the ileocecal region is most frequently involved [1], which is similar to our study in which we found 29.7% of GI lymphomas to be Burkitt’s lymphoma.
In a study by Somanath Padhi et al. [7] the central nervous system was the commonest site (29. 5%) of PENL, surpassing the GIT (25%). During our study period, we found only 4 patients (3.88%) with CNS lymphoma.
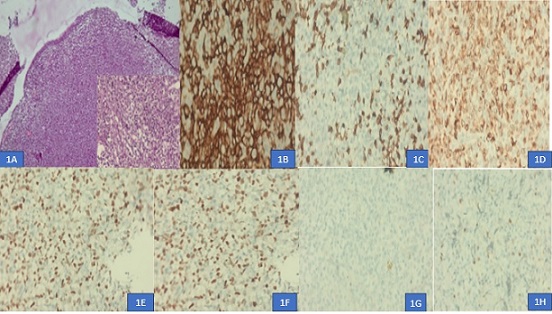
The head and neck region has been reported to be the most common site of origin of PENL in various studies from different parts of China (Yang et al., 2011)[8], India (Singh et al. 2003 ) [9] and Japan (Fujita et al. 2009 ) [10]. In our study, most head and neck lymphomas were nodal, and 7% were extranodal lymphomas, which is lower than that reported in other studies. There were two cases each of DLBCL and MZL and one case each of plasmablastic lymphoma and extranodal NK/T-cell lymphoma nasal type (Figure 1).
Figure 1. Nasopharyngeal DLBCL (GCB type). 1A, Atypical Lymphoid Cells in Sheets with Overlying Normal Epithelium. 1B, CD 20 positive b cells ( 400x). 1C, CD 3 positive in surrounding T cells. 1D, BCL2 positivity (400x), 1E, Ki67 positivity 70 % (400x). 1F, BCL 6 positive (400x). 1G,CD 10 negative (400x). 1H, MUM 1 negative (400x).
We reported a case of non-Hodgkin lymphoma of the thyroid with a background of Hashimoto’s thyroiditis in a 50-year-old female. Clinically, she complained of difficulty in deglutition. On fine-needle aspiration, the possibility of an NHL was considered, and in the resected specimen, the differential diagnosis included small cell variants of medullary carcinoma, insular carcinoma, and lymphoma. The tumor was negative for calcitonin, but positive for LCA and CD20, indicating lymphoma of the B-cell lineage.
Primary breast lymphoma (PBL) is a rare malignancy that accounts for less than 3% of extranodal lymphomas, 1% of non-Hodgkin’s lymphomas (NHLs), and 0.5% of all breast malignancies [11-13]. In this study, there were 16 cases of PBL. The majority of breast lymphomas were DLBCL, one case was follicular lymphoma, and one was mantle cell lymphoma.
Testicular lymphomas account for 5% of all testicular malignancies [14]. In our study, a single patient who was diagnosed with seminoma outside and on review was diagnosed as lymphoma, The tumour was positive for LCA and CD20, suggesting a diagnosis of B-cell NHL. No lymph nodes were enlarged even after 6 months of follow-up, so a secondary lymphoma was ruled out. After a panel of immunohistochemistry markers, we diagnosed it as DLBCL ABC type.
Primary cutaneous lymphomas are defined as non-Hodgkin lymphomas that are present in the skin with no evidence of extracutaneous disease at the time of diagnosis [15]. In our study, 10% of the patients had primary cutaneous lymphoma, 70% of whom had T-cell lymphoma. Among the CTCLs, the most common was primary cutaneous T-cell lymphoma NOS (PTCL NOS), followed by primary cutaneous ALCL and ALK-positive ALCL. Typically, there is sheet-like growth of tumour cells in the dermis, which may extend into the subcutaneous tissue, without significant epidermotropism. The tumour cells expressed CD30 (> 75% of tumor cells), and CD4, with variable expression of the T-cell antigens CD2, CD3, and CD5.
Most of the patients in the pENL group were diagnosed to have Stage I/II lymphoma whereas Stage III/IV was more common in patients with nodal NHL. Most of the patients were treated with chemotherapy following the diagnosis. The most common chemotherapy used was cyclophosphamide, doxorubicin, vincristine, and prednisolone regimen, and rituximab was a part of chemotherapy.
In conclusion, primary extranodal lymphomas constitute a diverse group of haematolymphoid malignancies. The diagnosis is a frequent challenge for pathologists, due to their morphological characteristics and varied clinical presentations. Immunohistochemistry plays a major role in the diagnosis of primary extranodal lymphoma. Compared to the published series, no difference was noted regarding sex predilection or morphology. However, as this was mostly an epidemiological and morphological study, data about the detailed therapeutic outcomes are lacking.
Abbreviations
pENL: Primary extranodal lymphoma, ALK: Anaplastic lymphoma kinase, DLBCL: Diffuse Large B Cell Lymphoma, GIT: Gastrointestinal tract, MZL: Marginal Zone lymphoma.
Acknowledgments
None
Conflict of Interest
The authors declare no conflict of interest.
Funding
No specific funding was received for this study
References
- Primary extranodal B-cell lymphoma: current concepts and treatment strategies Vannata B, Zucca E. Chinese Clinical Oncology.2015;4(1). CrossRef
- Epidemiology of non-Hodgkin's lymphoma (NHL): trends, geographic distribution, and etiology Müller AMS , Ihorst G, Mertelsmann R, Engelhardt M. Annals of Hematology.2005;84(1). CrossRef
- Primary testicular lymphoma Vural F, Cagirgan S, Saydam G, Hekimgil M, Soyer NA , Tombuloglu M. Journal of the National Medical Association.2007;99(11).
- Morphological Typing of Extranodal Lymphoma with Immunohistochemical Study Dhumure KS , Hanmante RD , Chopade SW , Bindu RS , Rajharsh D, Hanmante D. .
- Primary intestinal non-Hodgkin's lymphoma: a clinicopathologic analysis of 81 patients Wang G, Xu Gu, Luo G, Shan H, Li Y, Gao X, Li J, Zhang R. World Journal of Gastroenterology.2011;17(41). CrossRef
- Primary extranodal non-Hodgkin's lymphoma (NHL): the impact of alternative definitions tested in the Comprehensive Cancer Centre West population-based NHL registry Krol A. D. G., Cessie S., Snijder S., Kluin-Nelemans J. C., Kluin P. M., Noordijk E. M.. Annals of Oncology: Official Journal of the European Society for Medical Oncology.2003;14(1). CrossRef
- Primary extra nodal non Hodgkin lymphoma: a 5 year retrospective analysis Padhi S, Paul TR , Challa S, Prayaga AK , Rajappa S, Raghunadharao D., Sarangi R. Asian Pacific journal of cancer prevention: APJCP.2012;13(10). CrossRef
- Subtype distribution of lymphomas in Southwest China: analysis of 6,382 cases using WHO classification in a single institution Yang Q, Zhang W, Yu J, Zhao S, Xu H, Wang W, Bi C, et al . Diagnostic Pathology.2011;6. CrossRef
- Primary extranodal non-Hodgkin's lymphoma in northern India Singh D, Kumar L, Goyal H, et al . Proc Am Soc Clin Oncol.2003;22:2457.
- Features of primary extranodal lymphoma in Kanagawa, a human T-cell leukemia virus type 1 nonendemic area in Japan Fujita A, Tomita N, Fujita H, Motohashi K, Hyo R, Yamazaki E, Hattori M, et al . Medical Oncology (Northwood, London, England).2009;26(1). CrossRef
- Primary Breast Lymphoma: Analysis of 55 Cases of the Spanish Lymphoma Oncology Group Franco Pérez F, Lavernia J, Aguiar-Bujanda D, Miramón J, Gumá J, Álvarez R, Gómez-Codina J, et al . Clinical Lymphoma, Myeloma & Leukemia.2017;17(3). CrossRef
- Primary Breast Lymphoma in the United States: 1975-2013 Thomas A, Link BK , Altekruse S, Romitti PA , Schroeder MC . Journal of the National Cancer Institute.2017;109(6). CrossRef
- Primary breast diffuse large B-cell lymphoma: a population-based study from 1975 to 2014 Jia Y, Sun C, Liu Z, Wang W, Zhou X. Oncotarget.2018;9(3). CrossRef
- Primary extranodal lymphomas - spectrum of distribution and morphology with immunophenotyping: A 3-year institutional study Renuka I, Rajani M, Sailabala G, Annapurna P, Aparna C. ResearchGate.2024.
- The 2018 update of the WHO-EORTC classification for primary cutaneous lymphomas Willemze R, Cerroni L, Kempf W, Berti E, Facchetti F, Swerdlow SH , Jaffe ES . Blood.2019;133(16). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times