Life after Treatment: A Comparative Study of Quality of life among Cervical and Female Oral Cavity Cancer Survivors
Download
Abstract
Background: Cervical cancer is one of the most prevalent gynecological malignancies, while oral cavity cancer is the leading head and neck cancer. Advances in treatment have improved survival rates, but the long-term side effects significantly impact survivors’ quality of life (QoL). Understanding and comparing these impacts is crucial for post-treatment care.
Objective: This study aims to assess and compare the QoL of cervical and female oral cavity cancer survivors, identifying the most affected dimensions of their well-being.
Methods: A cross-sectional study was conducted at Vydehi Institute of Medical Sciences and Research Centre, Bangalore, involving 72 female cancer survivors (36 cervical, 36 oral cavity). QoL was assessed using the European Organization for Research and Treatment of Cancer (EORTC) QLQ-C30, along with disease-specific modules (Cx24 for cervical cancer, OH-14 and H&N-35 for oral cavity cancer). Statistical analysis included independent sample t-tests, Chi-square tests, correlation analysis, and ANOVA.
Results: Oral cavity cancer survivors exhibited significantly lower physical functioning (85.97 vs. 91.52, p = 0.047), role functioning (p = 0.024), and emotional functioning (p = 0.043) compared to cervical cancer survivors. Fatigue (p = 0.025), pain (p = 0.001), and diarrhea (p < 0.001) were significantly worse in oral cavity cancer survivors. The analysis of disease-specific QoL modules revealed that the oral cavity cancer survivors had more challenges with swallowing, speech, social eating, and pain management, whereas cervical cancer survivors faced significant issues with menopausal symptoms, peripheral neuropathy, and sexual well-being.
Conclusion: Survivors of oral cavity cancer experience a greater decline in QoL compared to cervical cancer survivors, particularly in physical and emotional domains. These findings emphasize the need for tailored post-treatment interventions to address the specific challenges faced by each group, improving long-term survivorship outcomes.
Introduction
Cervical cancer is one of the most widespread gynecological malignancies in women worldwide. Carcinoma cervix is the second most common type of cancer in the world. Treatment strategies and screening modalities have largely evolved in the past years resulting in an improvement of survival. However, treatment modalities are associated with long term side effects that significantly impacts quality of life (QOL) in cervical cancer survivors [1]. Survivorship continues to require attention and possible follow-up care. Cancer of the oral cavity is one of the most common cancers of the head and neck, and is one of the ten most common causes of death in the world. In the majority of cases, cancer of the oral cavity is detected in an advanced stage when therapeutic options are reduced, and the prognosis is much worse [2]. Persistent infection with oncogenic HPV types significantly contributes to the development of cervical cancer and certain oral cavity cancers.
Quality of life (QOL) is an important parameter to evaluate and modify in patients’ treatment. Quality of life among cancer survivors is a complex concept that includes various aspects of well-being, such as physical health, emotional balance, social connections, and overall life satisfaction. With improving survival rates for many cancers, research and healthcare are increasingly focusing on understanding and enhancing survivors’ quality of life. Assessing quality of life is an important indicator of the success of multidisciplinary treatment and highlights areas where the survivor may need additional support. This shift in focus aims to ensure that survivors not only live longer but also enjoy a better quality of life, addressing their comprehensive needs and fostering overall well-being in the long term.
Objective
1. To assess the quality of life among women after cervical cancer treatment.
2. To assess the quality of life among women after oral cancer treatment.
3. To compare the quality of life among the women with cervical and oral cancer after treatment.
4. To identify the specific dimensions of quality of life (physical, emotional, social, and functional) most impacted in each survivor group.
Materials and Methods
This is a type of cross-sectional study done in Vydehi hospital, a tertiary care hospital in Whitefield, Bangalore. Study population were the women treated for cervical and oral cancer with a sample size of 36.The sample size was calculated based on an expected mean difference of 6.9 between groups, a standard deviation of 9.6, a desired power of 0.80, and a significance level of 0.05, the minimum required sample size was calculated to be 31 participants per group. Using a power of 0.80 and a two-sided α of 0.05, sample size was calculated as:
n = 2 * (Zα/2 + Zβ) ² * σ² / Δ²
Where: Zα/2=1.96(for α=0.05)
Zβ=0.84(for 80% power)
n=2*(1.96+0.84)²*9.6²/6.9²
n=30.4
To account for potential dropouts and incomplete data, this was increased by 15%, resulting in a target sample size of 36 participants per group, or 72 participants total (36 cervical cancer survivors and 36 female oral cavity cancer survivors).
Selection criteria for the study: The inclusion criteria were:
A. Females 18 years and older
B. Were willing to participate in the study
C. Diagnosed with either cervical cancer at different stages (I, II or III), or oral cavity cancer
D. Have completed treatment for cervical and oral cancer 3 months before the start of the study. (Time expected for the appearance of medium and long term side effects).
The exclusion criteria were:
A. Not meeting the inclusion criteria
B. Didn’t consent for the study
C. Didn’t respond to call
D. Had recurrent disease at the time of recruitment
E. Critically ill patients
F. Had other comorbidities
G. Patient with cognitive and /or neurological deficit
H. Patients with ongoing active treatment for cancer
Data was collected from the list of the women treated for cervical and oral cancer (obtained from hospital cancer registry).
Participants were called over phone and assessed if they are eligible to participate in the study. Eligible participants were interviewed after obtaining informed consent. Interview (Questionnaire) contained sociodemographic details followed by questions on quality of life from EORTC (European Organization for Research and Treatment of Cancer) questionnaire (QLQ)-30, its Cervical cancer module (Cx24), Oral health module (OH-14), Head and neck cancer (H&N-35) and Head and neck cancer (update of QLQ-H&N43) modules encompassing physical, psychological, social and environmental domains and were also asked about oral hygiene practices and oral clinical parameters.
European Organization for Research and Treatment of Cancer quality of life questionnaire (EORTC QLQ-30) was used to assess quality of life in different types of cancer. It consisted of 30 questions assessing 15 scales: 5 functional scales (physical, emotional, social, role and cognitive function), 1 general health/ QoL scale, 3 symptom scales (fatigue, pain and nausea and vomiting), as well as several aspects and symptoms common in cancer patients (dyspnea, insomnia, loss of appetite, constipation, diarrhea and financial difficulties). For each question, a score from 1 to 4 was assigned, except for the general health subscale, which was scored from 1 to 7. In terms of interpretation, the results were transformed into scores from 0 to 100. A high score, greater than 75, indicated a better perception of quality of life while those patients with values less than or equal to 75 were classified as patients with low quality of life. For the five functional scales and the general quality of life scale a high score meant a good level of functionality. For the symptom scales, high scores were related to higher symptom severity [3, 4].
The head and neck cancer module incorporated seven multi-item scales that assess pain, swallowing, senses (taste and smell), speech, social eating, social contact, and sexuality. There were also eleven single items. For all items and scales, high scores indicated more problems (i.e. there were no function scales in which high scores would mean better functioning). The scoring approach for the QLQ H and N-35 was identical in principle to that for the SSs/single items of the QLQ C-30 [4, 5].
The participant information (such as name and contact details) were excluded to maintain confidentiality.
Plan of analysis/Statistical tools
Data was entered in MS Excel and analyzed using SPSS version 23.Descriptive analysis of all the explanatory and outcome parameters was done using mean and standard deviation for quantitative variables. Frequency and proportions for categorical variables. Independent sample t test was used for finding the mean difference between the groups. Chi square test was used for finding the association between the categorical variables. Correlation was used for finding the relationship between the Quantitative variables. ANOVA was used for compararing the means of two or more than two groups. The level of significance was set at p<0.05.
Results
Our research included 36 patients with oral cavity cancer and 36 patients with cervical cancer who received treatment within the past 1–2 years. Among 36 of oral cavity cancer patients, majority were from rural areas (29) and mean age group of 57 years and all of them were married (36); among them 9 were widow and 1 divorced. Most (34) of them were illiterate and majority of them (30) out of 34 cases were betel nut chewers. Many had the habit from decades (25-30years). Betel nut chewing was also prevalent among educated people (2 of the 2 cases).Most of the cases were diagnosed at a later stage of the disease T4 (66%) and most common modality of treatment was surgery (27 cases-75%).
Among 36 of cervical cancer patients, majority were rural population (28) and mean age group of 51 years and all of them were married (36); among them 3 were widow and 1 divorced. Majority of them (30) were illiterate. Cancer status of most of them was Stage 3 (13 cases) (36.1%) [3A-2cases, 3A1-1case, 3C1-7cases, 3C2-3cases] and 12 were in stage 2 (27.8%) [2A1-1case, 2A2-1case, 2B-10cases] and radiotherapy alone and combined with chemotherapy was the most common method of treatment modality (75%) of cases and surgery was mostly used for localized stage (stage1).
The independent sample t test revealed significant differences between the groups for Physical functioning, Role functioning, Emotional functioning, Fatigue, Pain, Diarrhea (p < 0.05). These results indicated that these variables exhibit meaningful differences in their mean values across the groups, as supported by the confidence intervals that do not include zero. For the remaining variables (Global health status, Cognitive functioning, Social functioning, Nausea and Vomiting, Dyspnea, Insomnia, Appetite loss, Financial difficulties), there was no statistically significant difference between the groups (p > 0.05), suggesting that the group means for these variables were not distinct. In summary, the findings demonstrate that only a subset of the variables shows significant group differences, while others remain consistent across the groups.
There was a significant difference in functional scores between the groups as shown in Table 1.
| Independent Sample t Test | ||||
| t | df | P value | Mean Difference | |
| Global Health Status | -1.543 | 70 | 0.127 | -5.3194 |
| Physical Functioning | -1.991 | 70 | .047* | -5.55 |
| Role Functioning | -2.311 | 70 | .024* | -4.1278 |
| Emotional Functioning | -2.064 | 70 | .043* | -4.5722 |
| Cognitive Functioning | -1.275 | 70 | 0.206 | -1.85 |
| Social Functioning | -0.127 | 70 | 0.899 | -0.4667 |
| Fatigue | 2.283 | 70 | .025* | 7.0333 |
| Nausea And Vomiting | 1.357 | 70 | 0.179 | 1.3861 |
| Pain | 3.329 | 70 | .001* | 12.4833 |
| Dyspnea | 1 | 70 | 0.321 | 0.925 |
| Insomnia | 1.435 | 70 | 0.156 | 1.85 |
| Appetite Loss | 0.633 | 70 | 0.529 | 1.8528 |
| Diarrhoea | 35 | 70 | .000* | 7.7778 |
| Financial Difficulties | -0.466 | 70 | 0.643 | -1.85 |
*represent p< 0.05 considered as significant.
Significant Differences (p < 0.05) was found in physical functioning (Mean Difference = -5.55): Cervical cancer patients (Mean = 91.52) had significantly higher values when compared to oral cavity cancer patients (Mean = 85.97). Role and emotional functioning cervical cancer patients consistently had a perfect score (Mean = 100, Std. Dev. = 0), which was significantly higher than oral cavity cancer patients (Mean = 95.87 and 95.43, respectively). Fatigue (Mean Difference = 7.03): Oral cavity cancer patients (Mean = 9.07) had significantly higher values compared to cervical cancer patients (Mean = 2.04). Pain (Mean Difference = 12.48): Oral cavity cancer patients (Mean = 14.79) showed significantly higher values compared to cervical cancer patients (Mean = 2.31). Diarrhea (Mean Difference = 7.78): Oral cavity cancer patients (Mean = 7.78) showed significantly higher values when compared to cervical cancer patients (Mean = 0).
No-Significant Differences (p > 0.05) was found in global health status, cognitive functioning, social functioning, nausea and vomiting, insomnia, dyspnea, appetite loss and financial difficulties between the oral cavity cancer and cervical cancer groups, as indicated by the independent samples test. For these variables, the group means are relatively close, and the p-values were greater than the significance threshold.
The comparison between oral cavity cancer (Group 1) and cervical cancer (Group 2) reveals the following as shown in Table 2 and Figure 1:
| N | Mean | ||
| Global Health Status | 1 | 36 | 66.392 |
| 2 | 36 | 71.711 | |
| Physical Functioning | 1 | 36 | 85.969 |
| 2 | 36 | 91.519 | |
| Role Functioning | 1 | 36 | 95.872 |
| 2 | 36 | 100 | |
| Emotional Functioning | 1 | 36 | 95.428 |
| 2 | 36 | 100 | |
| Cognitive Functioning | 1 | 36 | 98.15 |
| 2 | 36 | 100 | |
| Social Functioning | 1 | 36 | 88.972 |
| 2 | 36 | 89.439 | |
| Fatigue | 1 | 36 | 9.069 |
| 2 | 36 | 2.036 | |
| Nausea And Vomiting | 1 | 36 | 1.386 |
| 2 | 36 | 0 | |
| Pain | 1 | 36 | 14.794 |
| 2 | 36 | 2.311 | |
| Dyspnea | 1 | 36 | 0.925 |
| 2 | 36 | 0 | |
| Insomnia | 1 | 36 | 1.85 |
| 2 | 36 | 0 | |
| Appetite Loss | 1 | 36 | 2.778 |
| 2 | 36 | 0.925 | |
| Constipation | 1 | 36 | 0 |
| 2 | 36 | 0 | |
| Diarrhoea | 1 | 36 | 7.778 |
| 2 | 36 | 0 | |
| Financial Difficulties | 1 | 36 | 10.175 |
| 2 | 36 | 12.025 |
Figure 1. Comparison of Functional Scores between Oral Cavity Cancer and Cervical Cancer in a Compound Bar Chart..

There was significant difference between the groups as shown in Table 3.
| t | df | P value | Mean Difference | |
| Global Health Status | -1.545 | 70 | 0.127 | -0.3194 |
| Physical Functioning | 1.857 | 70 | 0.068 | 0.1444 |
| Role Functioning | 2.311 | 70 | .024* | 0.125 |
| Emotional Functioning | 1.776 | 70 | 0.08 | 0.11111 |
| Cognitive Functioning | 1.276 | 70 | 0.206 | 0.0556 |
| Social Functioning | 0.125 | 70 | 0.901 | 0.0139 |
| Fatigue | 2.1 | 70 | .039* | 0.1861 |
| Nausea and Vomiting | 1.357 | 70 | 0.179 | 0.0417 |
| Pain | 3.331 | 70 | .001* | 0.375 |
| Dyspnea | 1 | 70 | 0.321 | 0.0278 |
| Insomnia | 1.435 | 70 | 0.156 | 0.0556 |
| Appetite Loss | 0.632 | 70 | 0.529 | 0.0556 |
| Financial Difficulties | -0.466 | 70 | 0.643 | -0.0556 |
*represent p< 0.05 considered as significant.
The analysis revealed statistically significant differences between the groups for role functioning, fatigue and pain (p < 0.05) and supported by confidence intervals that do not include zero. For the remaining variables (global health status, physical functioning, emotional functioning, cognitive functioning, social functioning, nausea and vomiting, insomnia, dyspnea, appetite loss and financial difficulties) no significant differences were observed (p > 0.05), indicating that the raw scores for these measures are comparable between the groups.
The group statistics provided insights into the mean scores and variability between oral cavity cancer (Group 1) and cervical cancer (Group 2) for various variables as shown in Table 4 and Figure 2.
| N | Mean | ||
| Global Health Status | 1 | 36 | 4.986 |
| 2 | 36 | 5.306 | |
| Physical Functioning | 1 | 36 | 1.406 |
| 2 | 36 | 1.261 | |
| Role Functioning | 1 | 36 | 1.125 |
| 2 | 36 | 1 | |
| Emotional Functioning | 1 | 36 | 1.1111 |
| 2 | 36 | 1 | |
| Cognitive Functioning | 1 | 36 | 1.056 |
| 2 | 36 | 1 | |
| Social Functioning | 1 | 36 | 1.333 |
| 2 | 36 | 1.319 | |
| Fatigue | 1 | 36 | 1.247 |
| 2 | 36 | 1.061 | |
| Nausea And Vomiting | 1 | 36 | 1.042 |
| 2 | 36 | 1 | |
| Pain | 1 | 36 | 1.444 |
| 2 | 36 | 1.069 | |
| Dyspnea | 1 | 36 | 1.028 |
| 2 | 36 | 1 | |
| Insomnia | 1 | 36 | 1.056 |
| 2 | 36 | 1 | |
| Appetite Loss | 1 | 36 | 1.083 |
| 2 | 36 | 1.028 | |
| Constipation | 1 | 36 | 1 |
| 2 | 36 | 1 | |
| Diarrhoea | 1 | 36 | 1 |
| 2 | 36 | 1 | |
| Financial Difficulties | 1 | 36 | 1.306 |
| 2 | 36 | 1.361 |
Figure 2. Comparison of Raw Scores between Oral Cavity Cancer and Cervical Cancer in a Compound Bar Chart..
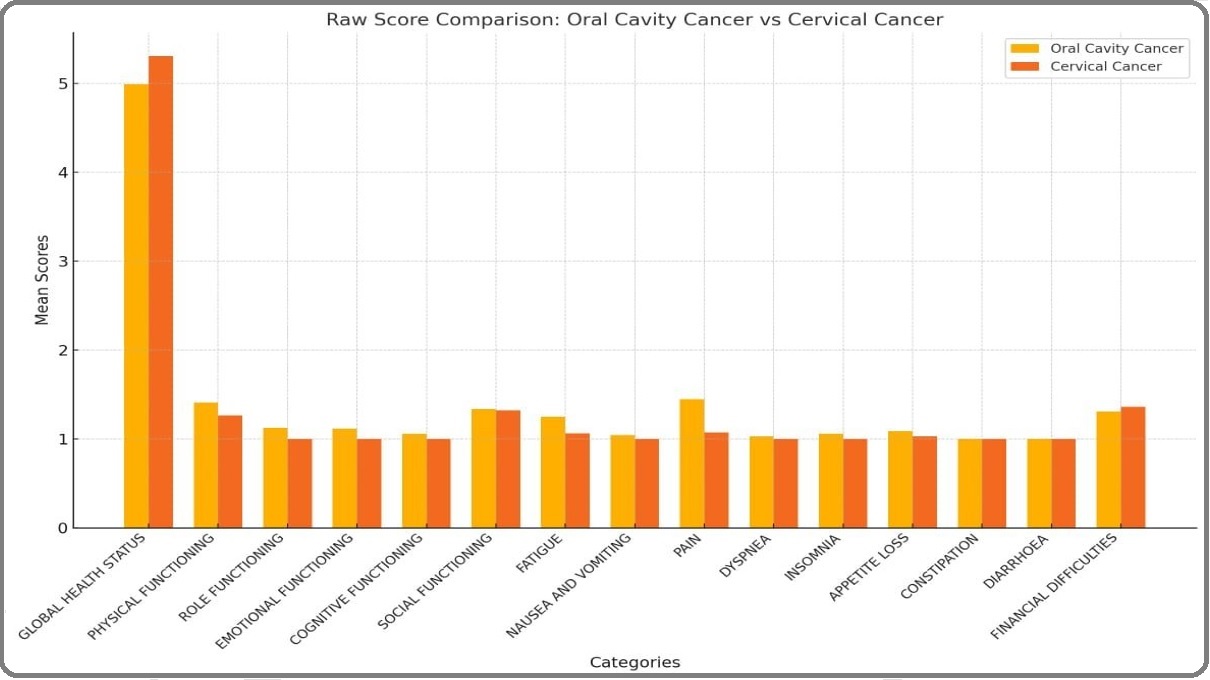
Significant differences was found in role functioning of oral cavity cancer patients (Mean = 1.125). Oral cavity cancer higher scores than cervical cancer patients (Mean = 1.0, Std. dev = 0). Fatigue among oral cavity cancer patients (Mean = 1.247) had higher scores compared to cervical cancer patients (Mean = 1.061). Pain among oral cavity cancer patients (Mean = 1.444) had significantly higher scores compared to cervical cancer patients (Mean = 1.069).
No Significant Differences was found in global health status, physical functioning, emotional functioning, cognitive functioning, social functioning, nausea and vomiting, insomnia, dyspnea, appetite loss and financial difficulties. Variables showed overlapping means or minimal differences between the groups, supported by the lack of statistical significance in the independent samples test. For diarrhea and constipation standard deviations are zero for both groups, making statistical testing infeasible. This indicated identical scores for all participants in these variables.
For oral health questionnaire the variables showed measurable variability in Oral health related quality of life, sticky saliva, and sensitivity, with Oral health related quality of life showed moderate variability (Mean = 1.2442) and sticky saliva and sensitivity had slight variability (Means of 1.056 and 1.083, respectively) and other variables showed no variability were sore mouth and dentures across all observations.
For oral cavity cancer QLQ-HN43 questionnaire the variables showed significant variability were swallowing, opening mouth, speech, social eating, and pain killer usage, and variables with minimal or no variability are teeth, sexuality, weight loss, and weight gain ,with many values clustered around 0.
For cervical cancer CX-24 questionnaire the variables showed significant variability were symptom experience, peripheral neuropathy, menopausal symptoms, and sexual worry and variability with minimal variability are body image, lymphedema, and sexual activity. The frequency table showed a uniform response of ‘No’ for all observations, indicating no variability in those categorical variables.
Discussion
There were significant differences between the two groups (oral cavity cancer and cervical cancer) in several aspects of their functional scores. Specifically, significant differences were found in: Physical Functioning (p = 0.047), Role Functioning (p = 0.024), Emotional Functioning (p = 0.043), Fatigue (p = 0.025), Pain (p = 0.001), Diarrhea (p = 0.000).
These results suggest that the patients with oral cavity cancer and cervical cancer experienced distinct differences in their functional health status, with some areas like pain and fatigue showing particularly pronounced differences. Other variables, such as global health status, cognitive functioning, and social functioning, did not show significant differences.
In the comparison between oral cavity cancer (1) and cervical cancer (2), the results indicated that oral cavity cancer (1) had a more significant impact on the quality of life, as it shows greater impairments in several functional areas. Specifically, oral cavity cancer patients experience more severe challenges in Physical Functioning, Role Functioning, Emotional Functioning, Fatigue, Pain, and Diarrhea, with statistically significant differences in these domains (p < 0.05). This suggests that oral cavity cancer had a more pronounced effect on the patients’ overall health and well-being compared to cervical cancer.
In a research done on Arab whites, it was found that long term cervical cancer score have generally a good global QOL comparable with healthy controls [1].
However, issues concerning cervical cancer; cervical cancer patients experienced less sexual functioning and enjoyment and less satisfaction with their body image when compared to healthy controls and research in tertiary care hospital in Ghana also showed that 75% of the survivors had a good overall quality of life and loss of appetite, pain or diminution in body image perception predicted the overall quality of life of cervical cancer survivors after treatment [6]. Our research showed that Symptom experience, peripheral neuropathy, menopausal symptoms, and sexual worry had significant effect on quality of life of survivors of cervical cancer patients.
An article about quality of life among oral cavity cancer survivors also showed that the clinical manifestations of oral cancer and the effects of treatment can have a negative impact on a patient’s quality of life. Physiological functions, cosmetic appearance, and psychological well-being can become compromised during the diagnosis, treatment, and survivorship of patients with oral cancer and a prospective study on quality of life of oral cavity cancer in China also showed that levels of pain, mood, and anxiety showed clinically and statistically significant improvements between diagnosis and at 8 years following treatment, whereas problems with chewing, speech, shoulder mobility, and taste worsened during this interval (P < .05) [7, 8]. Our research showed that swallowing, opening mouth, speech, social eating, and pain killer usage exhibited notable variability among oral cavity cancer patients.
QOL not only refers to how long patients survive but also stresses social function and mental status, emphasizes subjective feelings and functional status, and reflects individual or population health condition from multiple scales [9].
QOL consideration plays a significant role in exploring pertinent precautions and in evaluating the quality of medical health service. It also meets the novel medical goal proposed by WHO: prevent and treat disease, prolong survival, increase QOL, reduce death rate, and promote mental and physical health.It is important to provide preoperative psychological reassurance to increase postoperative adaptation in dealing with psychosocial difficulties, such as feeling of hopelessness and psychological distress resulting from physical handicaps and subsequent to significant life changes [10]. Although numerous studies have examined the quality of life among survivors of oral cavity cancer and cervical cancer individually, comparative research between these two groups remains limited. This study seeks to address this gap by directly evaluating and comparing the quality of life outcomes among survivors of both cancer types.
In conclusion, the comparison between oral cavity cancer and cervical cancer revealed that oral cavity cancer had a more pronounced impact on patients’ quality of life, even when both are associated with HPV (Human papilloma virus) infection. Individuals with oral cavity cancer experienced greater challenges in various aspects of their health, including physical functioning, emotional well-being, pain, fatigue, and gastrointestinal issues. These factors contributed to a more profound disruption in daily activities and overall health. As a result, patients with oral cavity cancer faced more severe impairments, highlighting the need for tailored care and support to address these specific challenges and improve their quality of life.
Acknowledgements
I extend my sincere gratitude to Vydehi Institute of Medical Sciences and Research Centre and department of Oncology, for providing the necessary resources and support for this study, the institution’s commitment to research and patient care has been instrumental in facilitating our work.
My heartfelt thanks also goes to the patients who participated in this study, sharing their experiences and contributing to a deeper understanding of survivorship and quality of life. Additionally, I extend my gratitude to the hospital’s medical and research staff for their cooperation and assistance.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
Conflict of interest
The authors declare no conflict of interest.
References
- Impact of cervical cancer on quality of life: beyond the short term (Results from a single institution): Quality of life in long-term cervical cancer survivors: results from a single institution Khalil J., Bellefqih S., Sahli N., Afif M., Elkacemi H., Elmajjaoui S., Kebdani T., Benjaafar N.. Gynecologic Oncology Research and Practice.2015;2. CrossRef
- Quality of Life of Patients with Oral Cavity Cancer Dzebo S, Mahmutovic J, Erkocevic H. Materia Socio-Medica.2017;29(1). CrossRef
- Quality of life in long term survivors of cervical cancer: A cross sectional study Shylasree T. S., Ranade R, Kattepur AK , Kaur S, Dusane R, Maheshwari A, Mahantshetty U, et al . Indian Journal of Cancer.2021;58(2). CrossRef
- Assessment of quality of life of patients 1-5 years after treatment for oral cancer Khandelwal A, Neeli A, Gadiyar A, Khandelwal A. Indian Journal of Dental Research: Official Publication of Indian Society for Dental Research.2017;28(5). CrossRef
- Quality of Life Assessment With European Organisation for Research and Treatment of Cancer Questionnaire (Head and Neck Module 43) and Its Clinicopathological Correlation Among Patients Treated for Oral Squamous Cell Carcinoma: An Exploratory Study Ramalingam K, Krishnan M, Ramani P, Muthukrishnan A. Cureus.2023;15(2). CrossRef
- Health-related quality of life among cervical cancer survivors at a tertiary hospital in Ghana Amo-Antwi K, Agambire R, Konney TO , Nguah SB , Dassah ET , Nartey Y, Appiah-Kubi A, et al . PloS One.2022;17(6). CrossRef
- Impact of Oral Cancer on Quality of Life Valdez JA , Brennan MT . Dental Clinics of North America.2018;62(1). CrossRef
- Quality of life in long-term oral cancer survivors: an 8-year prospective study in China Yan Y, Meng L, Liu Z, Xu J, Liu H, Shen J, Zhang X, Peng X, Mao C. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2017;123(1). CrossRef
- Assessment of quality of life for the patients with cervical cancer at different clinical stages Xie Y, Zhao F, Lu S, Huang H, Pan X, Yang C, Qiao Y. Chinese Journal of Cancer.2013;32(5). CrossRef
- Psychosocial responses to oral and maxillofacial surgery for head and neck cancer Strauss R. P.. Journal of Oral and Maxillofacial Surgery: Official Journal of the American Association of Oral and Maxillofacial Surgeons.1989;47(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times