A Rare Case Series of Vaginal Melanoma- experience of National Cancer Institute Sri Lanka
Download
Abstract
Vaginal melanomas are extremely rare gynaecological malignancy with aggressive behavior resulting in poor outcome. The aetiology is not well understood so far. There is no standardized treatment owing to the extreme rarity of the disease, however surgical excision with adjuvant radiotherapy has been the widely practiced treatment. The role of lymphadenectomy is controversial. The six cases reported between November 2015 to November 2021 at the National cancer institute Sri Lanka were treated primarily by surgical excision including hysterocolpectomy, colpectomy, and wide local excision. Pelvic lymphadenectomy was not done in most cases. Only one patient has received adjuvant radiotherapy. Only one patient died during the follow-up and 2 had recurrences.
Introduction
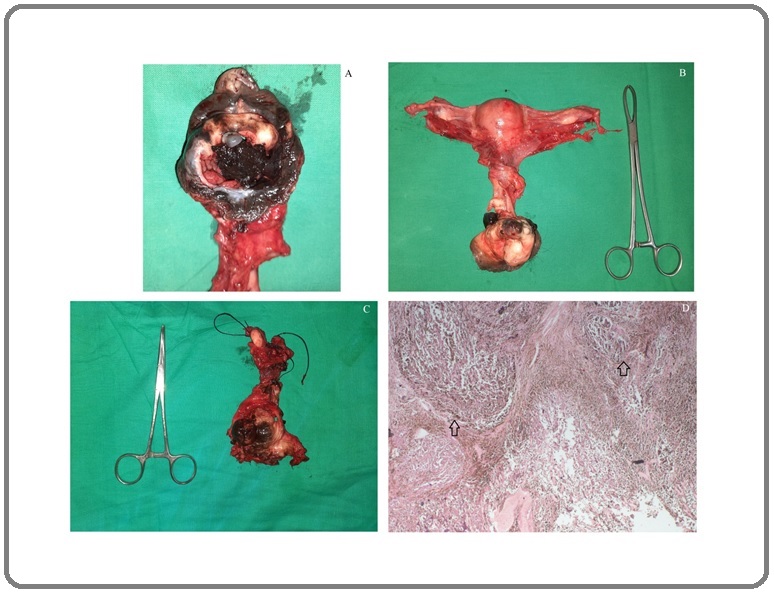
Cutaneous melanomas commonly affect keratinising squamous cell epithelium of sun-exposed skin and are usually detected in the early-stage owing to its location and resulting in a relatively good prognosis [1]. However gynaecological melanomas are rare and outcomes are poor compared to cutaneous melanomas [2]. Vaginal melanomas are even rare gyanecological malignancy with an incidence of 3 per 10 million women per year [3]. The two different nature of behaviours and the aetiology are not well understood [4]. The usual presentation is around age of 60 years [5]. Postmenopausal bleeding, irregular menstrual bleeding, pain, vaginal growth and vaginal discharge are the common symptoms [1]. Commonly the tumors are unifocal in nature [6] and appear as black color growth. Microscopically, malignant oval cells of melanoma in clusters heavily laden with dark brown pigments can be seen (Figure 1).
Figure 1. A-Macroscopic Appearance of Vaginal Melanoma. B-Specimen of hysterocolpectomy showing the uterus and vagina C-Specimen of colpectomy showing the vagina. Knot at the upper end of the vagina. D-Microscopic view of vaginal melanoma. Arrow indicates malignant oval cells of melanoma in clusters heavily laden with dark brown pigments.
The primary surgery is the mainstay of the treatment, and the extent of surgery ranges from more conservative wide local excision to more radical approaches including hysterocolpectomy, total or partial colpectomy (vaginectomy) and exenterative procedures in advanced stages [6,7]. Topical imiquimod, radiotherapy, chemotherapy and immunotherapy (interferon alpha) have been used as adjuvant treatment in case studies [8]. Lungs, liver, bone, and brain are the common sites of metastases [9].
Maerials and Methods
From November 2015 to November 2021, six patients diagnosed with vaginal melanomas were treated at National Cancer Institute. Their clinical records, surgical findings, and histology profiles were analyzed.
Results
The mean age of the patients was 65.1 years (Range 43- 77 years) and all were parous. Five patients presented with post-menopausal bleeding while the only premenopausal patient had vaginal discomfort and a vaginal growth. None of the patients had a history of familial gynaecological malignancies and 3 patients had prior hysterectomies for benign causes.
Hystero-colpectomy, colpectomy, and wide local excision (WLE) were done in 2 patients each. In cases where the hystero-colpectomy was carried out, bilateral salpingo-oophorectomy also had been performed (Table 1).
| Patient number | Age | Ethnicity | Parity | PMH | Menopausal state | Past Surgery | Surgery | Lymphadenectomy | Chemotherapy | Radiotherapy | Follow up | Follow up duration |
| 1 | 77 | S | 5 | No | Yes | No | Hysterocolpectomy | No | No | No | Uneventful | 9m |
| 2 | 77 | S | 5 | No | Yes | No | Hysterocolpectomy | No | No | No | Urinary incontinence. Lung deposit. | 6m |
| 3 | 63 | S | 2 | No | Yes | TAH | Colpectomy | No | Yes | Yes | Died | 38m |
| 4 | 69 | S | 2 | HTN DL | Yes | VH&R | Colpectomy | PND GND | No | No | Post-operative L LL DVT | 4m |
| 5 | 62 | S | 2 | BA DL HypoT | Yes | TAH BSO | Vaginal wall polypectomy & WLE. Re-excision done | No | No | No | Uneventful | 44m |
| 6 | 43 | M | 1 | HypoT | No | No | WLE- anterior vagina | FNAC nodes | No | No | Defaulted. Recurrence 46 months later. | 49m |
With regard to the lymph node dissection, only one patient underwent pelvic and groin node dissection and found to have negative for tumor cells and another patient who had WLE, underwent fine-needle aspiration cytology (FNAC) of ultrasonically enlarged nodes also found negative for tumor cells. Only one patient who had WLE had to undergo re-excision due to the involvement of the deep resection margins in the histology.
Mean follow-up was 25 months (Range 4-49 months). Except for one, all others are alive and on follow-up. With regard to the surgical morbidity, one hystero- colpectomized patient has true urinary incontinence and is kept on an indwelling urinary catheter following failed medical and surgical measures. The patient who had colpectomy and lymphadenectomy developed left lower limb deep vein thrombosis in postoperative 4th day and had successful thrombolysis.
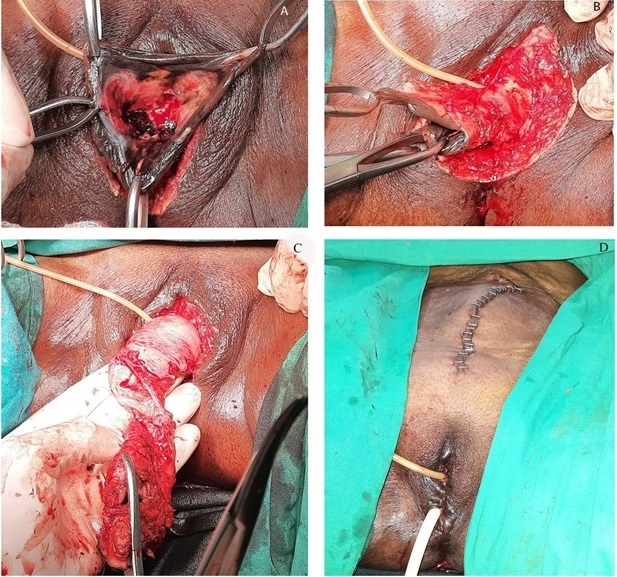
The youngest patient of all has defaulted to the follow-up and the adjuvant treatment. She presented 46 months after initial WLE complaining of right lower limb numbness and revealed to have metastatic deposits of pelvic lymph nodes resulting in palpable pelvic mass up to mid umbilicus (Figure 2).
Figure 2. Abdominal Recurrence of Melanoma A-Right Ovary with Deposits of Melanoma B-Black Melanocytic Materials in Left Adnexa C-Debulked Tumor Deposits of Lymph Nodes and Specimen of Uterus and Ovaries.

She was planned for palliation following palliative hysterectomy and bilateral salpingo- oophorectomy without lymphadenectomy.
The only patient who died during the follow-up was one who had colpectomy at the age of 63. She received adjuvant radiotherapy. Five months later she was diagnosed with papillary carcinoma of the thyroid and underwent total thyroidectomy. When she passed away 38 months after the initial surgery, she had multiple lung and brain metastasis despite radioactive iodine and chemotherapy.
Although 2 patients were planned for adjuvant radiotherapy, only one has received the complete course since the other patient has defaulted. Three patients were not planned adjuvant radiotherapy considering the age, performance status, and adverse effects. One WLE patient was not offered adjuvant treatment.
Discussion
Vaginal melanomas are extremely rare. It is commonly observed in patients with advanced age and except for one patient who was 43 years old, all others were above 60 years in this series. Ethnic or geographic variation was not very clear as most were Sinhalese and they were from different parts of the country. Although medical comorbidities were not significant with regard to non- communicable diseases, 3 had thyroid-related conditions including papillary thyroid carcinoma. Large case numbers are needed to correlate any relationship between them. The commonest presenting symptom was post-menopausal bleeding.
Surgical excision was the mainstay of the primary treatment ranging from more conservative WLE to more radical approaches of colpectomy or hysterocolpectomy.
Hysterocolpectomy was performed as a combined abdomino-vaginal procedure where the abdominal approach involves hysterectomy similar to the radical hysterectomy to dissect up to the mid vagina and the vaginal approach completed the total excision of the vagina (Figure 3) [7].
Figure 3. A Surgical Steps of the Vaginal Approach of Hysterocolpectomy. A-Incision of lower vaginal margin. B-dissecting the lower vagina. C- Delivering the uterus through introitus. D- Immediate post-surgical appearance.
Salpingo-oophorectomy was performed if not done before. Omentectomy was not done and none of the primary cases revealed macroscopic peritoneal metastatic deposits. Whether to do routine pelvic or groin node dissection was not standardized [10] and, here only one patient had bilateral pelvic and groin node dissection and found negative for lymph node metastasis. FNAC in another patient was also found negative. Colpectomy was the option for those who had a hysterectomy before.
True urinary incontinence following hysterocolpectomy is likely to occur since the lower urethra is excised and due to the possible damage to the urethral sphincter in the weak pelvic floors of the menopausal patient. Surgical or medical measures were failed to resolve her symptoms and she was inserted on an indwelling urinary catheter. DVT in the immediate post-operative period is likely due to extensively radical pelvic surgery. Two other colpectomy patients had no significant surgical morbidity.
Since the papillary carcinoma of the thyroid is having low malignant potential [11], lung and cerebral metastasis are likely due to the melanoma in the only patient who died. Patient 2 (Table 1) had possible pulmonary metastasis in 6 months postoperatively and patient 6 (Table 1) had the recurrence in the pouch of Douglas forming a mass and with no tumor recurrence in the upper abdomen or lungs. In conclusion, vaginal melanomas are rare gynaecological malignancies with aggressive behavior. The prognosis is poor. Most patients presented with post-menopausal bleeding. Surgical excision had been performed in all cases as a primary treatment and lymphadenectomy was performed in only one case. One patient died during the follow up and 2 others also had recurrences.
Acknowledgements
The authors would like to acknowledge the Department of Pathology, National Cancer Institute, Maharagama; Dr (Mrs) PriyangieAmarabandu and Dr (Mrs) S.B.K. Gamage for providing the histology slides and explanations.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
The authors declare no conflict of interest.
References
- Review of gynaecological malignant melanomas Platt Sarah, Wilson Ewan, Pawade Joya, Walther Axel, Newton Claire. The Obstetrician & Gynaecologist.2020;22(3). CrossRef
- Management of advanced vaginal melanoma: a case report and review of the literature Orellana Taylor, Beriwal Sushil, L Kelley Joseph, P Edwards Robert, Sukumvanich Paniti, B Olawaiye Alexander. Clinical Obstetrics, Gynecology and Reproductive Medicine.2020;6(6). CrossRef
- Gynecologic Cancer InterGroup (GCIG) consensus review for vulvovaginal melanomas Mm Leitao, X Cheng, Al Hamilton, Na Siddiqui, I Jurgenliemk-Schulz, S Mahner, E Åvall-Lundqvist, K Kim, G Freyer. International journal of gynecological cancer : official journal of the International Gynecological Cancer Society.2014;24(9 Suppl 3). CrossRef
- Primary Malignant Melanoma of the Vagina without Metastasis: A Rare Case and Review of Literature Wilson Bizimana, Akimana Gloria, Insumbo Arthur, Jerguigue Hounayda, Latib Rachida, Omor Youssef. Asian Journal of Oncology.2020;7. CrossRef
- Factors affecting risk of mortality in women with vaginal cancer Ca Shah, Ba Goff, K Lowe, Wa Peters, Ci Li. Obstetrics and gynecology.2009;113(5). CrossRef
- Primary malignant melanoma of the vagina Frumovitz Michael, Etchepareborda Mariano, Sun Charlotte C., Soliman Pamela T., Eifel Patricia J., Levenback Charles F., Ramirez Pedro T.. Obstetrics and Gynecology.2010;116(6). CrossRef
- An extremely rare case of vaginal melanoma treated with hysterocolpectomy Wijeratne Y, Kannangara S. Journal of the Postgraduate Institute of Medicine.2021;8(2):1-6. CrossRef
- Cancer of the vagina Adams Tracey S., Cuello Mauricio A.. International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics.2018;143 Suppl 2. CrossRef
- Primary Vaginal Malignant Melanoma: A Case Report and Review of Literature Paravathaneni Mahati, Edlukudige Keshava Vinay, Baralo Bohdan, Thirumaran Rajesh. Cureus.2020;12(9). CrossRef
- A Case of Vaginal Malignant Melanoma Completely Resected by Radical Surgery R Tokumitsu, T Hirakawa, M Yano, E Kirakosyan, S Sato, K Nasu, H Narahara. The American journal of case reports.2020;21. CrossRef
- Papillary thyroid carcinoma: an update LiVolsi Virginia A.. Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc.2011;24 Suppl 2. CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times