Management of Lymphoepithelial Carcinoma of the Parotid Gland with Liver Metastasis: A Case Report
Download
Abstract
Objective: Lymphoepithelial carcinoma (LEC) is rarely found as one type of salivary gland malignancy, especially the parotid gland. Based on data only covers 0.86% of all cases of salivary gland malignancies with an annual incidence rate of 0.01 cases per 100,000 population. Liver metastasis from this type of cancer is very uncommon.
Methode: We reported a 64-year-old female patient who presented with a lump in the left neck which enlarged within four years. Total parotidectomy and modified radical neck dissection were done and the diagnosis of lymphoepithelial carcinoma of the parotid gland was establishes based on pathology examination. The patient was then given adjuvant radiotherapy. Five months after initial treatment, the patient shows no locoregional recurrence. However, the patient developed multifocal liver metastases which were deemed inoperable.
Results: Liver metastases in the case of lymphoepithelial carcinoma have a worse prognosis than other types of cancer because it usually manifests in multiple and disseminated lesions rather than solitary.
Introduction
Salivary gland malignancy is a relatively rare health problem. Cases of salivary gland malignancies cover less than 3% of head-neck malignancies with annual incidence rates ranging from 0.05-2 cases per 100,000 population [1, 2]. Most types of salivary gland malignancies are mucoepidermoid carcinoma, squamous cell carcinoma, adenoid cystic carcinoma, and non-specific adenocarcinoma [3, 4]. Lymphoepithelial carcinoma (LEC), a type of carcinoma with the pathological appearance in the form of squamous cell carcinoma accompanied by the presence of lymphoid stroma, only covers 0.86% of all cases of salivary gland malignancies with an annual incidence rate of 0.01 cases per 100,000 population [3, 5]. To our knowledge, only a few cases have been reported and this is the first case of lymphoepithelial carcinoma in the parotid gland with liver metastases documented from Indonesia.
Case Illustration
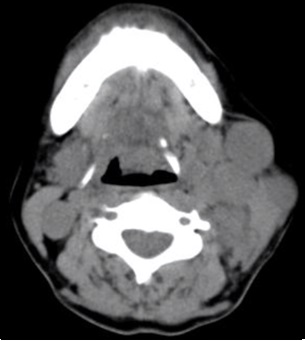
A 64-year-old woman presents with a hard lump in the left neck area that enlarges slowly within four years (Figure 1).
Figure 1. A 63-year-old Woman Complained of a Palpable Masses in the Neck Area.

Initially, there was only one lump but another lump appears within one year before the patient decided to go to the doctor. The patient denies a decrease in appetite, weight loss, difficulty in swallowing, or a feeling of tightness around the neck area. The patient complained of no pain at that time, and her facial nerve function was intact, with House-Brackmann grade I. Family history of cancer is denied. History of smoking or drinking alcohol is also denied. The patient also had no previous history of other head and neck cancer. Patient’s Karnofsky score was 80%, with physical examination shows no trismus nor hearing disorder. There were palpable lymph nodes in the submandibular area and posterior neck area. A computed tomography (CT) scan acquired at that time showed a hyperdense (compared to salivary gland) mass in the superficial lobe of the left parotid gland and multiple masses that conglomerates in the profound lobe of the parotid gland, suggesting enlarged lymph nodes (Figures 2 and 3).
Figure 2. A CT Scan Reveals a Left-sided Parotid Mass (superficial lobe) in the Axial Plane.

Figure 3. A CT Scan Reveals Left-sided Multiple Masses in the Profound Lobe of the Parotid in the Axial Plane.
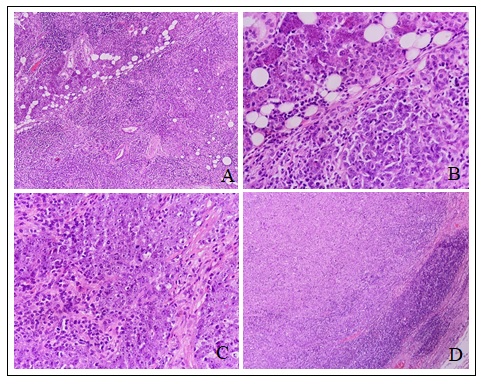
Total parotidectomy with preservation of facial nerve and modified radical neck dissection involving level I-V lymph nodes were performed in the patient, and postoperative pathology showed lymphoepithelial carcinoma and metastasis to neck lymph nodes level I-V (Figure 4).
Figure 4. A. The Tumor within Parotid Glands (HE, 100x). B. Nest of tumor and non-neoplastic lymphoid infiltrate (HE, 400x). C. Pleomorphic cells, vesicular, prominent nucleoli, eosinophilic cytoplasm, indistinct cell borders, high mitotic activity, dense lymphoid infiltrate (HE, 400x). D. Metastasis tumor into lymph nodes (HE, 40x).
Eight weeks after surgery the patient underwent radiation therapy in Intensity Modulated Radiation Therapy (IMRT) technique. The primary tumor bed, which is left parotid gland, was considered as high-risk Planning Target Volume (PTV). It received a 66 Gy dose of radiation whilst ipsilateral neck lymph nodes, considered as intermediate risk PTV, received 60 Gy in 33 fractions. Contralateral nodes were considered as low-risk PTV, and received 50 Gy in 33 fractions.
From the Dose Volume Histogram (DVH) of the radiation, the mean dose of the PTV for the primary tumor bed was 6690 cGy, PTV for ipsilateral node 6163 cGy, and the PTV for contralateral node is 5089,2 Gy. Patient’s hemoglobin level during irradiation series was considerably accepted, all were above 10 g/dL. Her performance status also generally good, with Karnofsky score above 70%.
At the fifth month of follow-up, the patient showed no locoregional recurrence but his general condition worsened, with Karnofsky score of 20%. Patient was submitted to inpatient care and during treatment the patient became jaundice, with markedly elevated bilirubin, AST, ALT, and significantly decreased albumin and platelets. Then a three-phase abdominal CT scan was performed with the results of hepatomegaly with multiple metastatic lesions in both lobes of the liver (Figure 5).
Figure 5. Abdominal CT Scan Shows Multiple Metastatic Lesions in both Lobes of Liver.
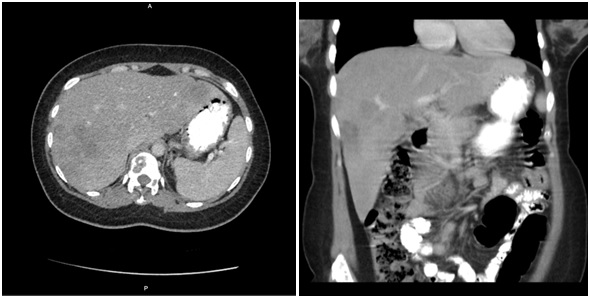
A week later patient died with the cause of liver failure.
Discussion
LEC is a type of carcinoma with a pathological appearance in the form of squamous cell carcinoma accompanied by the presence of lymphoid stroma. This type of malignancy is often found in the nasopharynx and very rarely found in other structures in the head and neck area, especially the salivary glands [5]. Patients with this type of malignancy are mostly over the age of fifty years old with women making up the bulk of the cases. This carcinoma is thought to be associated with Epstein-Barr virus (EBV) infection and is more commonly found in certain demographics such as East Asia, Southwest Asia, and the Arctic Circle [1, 5]. Alleged pathophysiology of this type of carcinoma is EBV infection in patients from certain demographics who have tumorigenesis predilection, triggering changes that cause tumor cells to develop [6]. However, some cases also report findings of this type of malignancy outside the endemic area; in some of these cases, EBV was not detected. This has led to the suspicion that there are other mechanisms involved in the pathophysiology of this type of malignancy in addition to EBV infection [7].
Patients with lymphoepithelial carcinoma in salivary glands generally present with complaints of a painless, unilateral mass that grows slowly. This complaint can be accompanied by enlarged lymph nodes (commonly occurs in 10-40 % of cases) or facial nerve paralysis [8, 9]. Imaging, such as ultrasonography and CT scan, plays an important role in establishing the diagnosis. In addition to showing the characteristics of lymphoepithelial carcinoma malignancy, it also shows the extent of the malignant tissue and its spread to other salivary glands or the surrounding lymph nodes [1, 10, 11]. Histopathological appearance of this type of carcinoma is generally in the form of the neoplastic epithelium of various sizes with interstitial infiltration in the form of lymphocytes and plasma cells [11, 12]. Immunohistochemistry examination is generally found to be positive for cytokeratin in the presence of CD3 and CD20 cell biomarkers [6].
Management of LEC of the parotid gland is total parotidectomy with or without neck dissection. Total parotidectomy is performed under conditions of tumors involving the profound lobe, malignant, and large size. Neck dissection needs to be considered if the accuracy of the staging at the preoperative or intraoperative stage is doubtful [6, 11, 13]. Postoperative radiotherapy is indicated for unfavorable prognostic features, such as close or positive surgical margins, high-grade malignancy, perineural invasion, tumor infiltration of adjacent organs, recurrent disease, and regional metastasis, and has been shown to improve locoregional control and increase survival. In addition to its role in killing tumors and microtumors that may be spilled during surgery, radiotherapy is chosen as adjunctive treatment because this type of carcinoma is known to be radiosensitive [1, 7, 14]. In this patient, en bloc resection of the tumor was performed with total parotidectomy because there were also masses found in the profound lobe of the parotid gland, and it has already metastasized to the neck lymph nodes. Hence the tumor is more likely to be malignant. Modified radical neck dissection was also performed because the patient had positive nodes clinically. We decided to give radiotherapy as an adjuvant for locoregional control. In general, we can assume that the radiation dose given to this patient is already adequate. However, there is prolonged window period for radiation time, following the surgery timeline. The patient received first radiation fraction more than 10 weeks after the resection due to pandemic issues and insurance matters.
During the irradiation, the patient experienced radiation-related side effects such as grade 1 radiodermatitis, grade 1 xerostomia, and mild mucositis. The patient still could get oral intake despite these signs. But within 6 weeks the patient’s body weight decreases by 7 kg due to nausea and bloating. According to history, the decline in general performance and complaints of nausea and bloating began during week 3 of irradiation, and we later learned that there was liver metastasis, which may have occurred earlier in the irradiation sequence.
The risk of remote metastases with bulky nodal disease is reported to be especially high in this case because radiotherapy only provides excellent local control. Lymphoepithelial carcinoma of salivary gland (LECSG) has histological characteristics identical to non-keratinizing undifferentiated carcinoma of the nasopharynx (UCNT), also known as WHO type III endemic nasopharyngeal cancer. They are also similar in terms of their relationship with EBV [15]. The rareness of the disease and the lack of prospective data make it difficult to evaluate the diagnostic approach, the prognostic factors, and the impact of different treatment modalities on the outcome of the patient. Also, the treatment protocol is not well established yet. Given that the cases about LECSG, especially those who metastasize to the liver are scarce, it might be useful to learn from its identical twin, which is UCNT. UCNT is a chemosensitive tumor. The neoadjuvant use of systemic chemotherapy for locoregional disease has been the topic of several studies over the last few years. Studies of induction chemotherapy indicate that UCNT, as shown by the high response rates, is highly responsive to pre-irradiation chemotherapy, namely between 10% and 66% of complete response (CR) and an objective response rate of 75-98%. The regimen used mostly is platinum-based [16].
In conclusion, Lymphoepithelial Carcinoma is a rare type of parotid tumor that requires surgical intervention and radiotherapy. Surgically, we recommend total parotidectomy and radical/modified neck dissection to all patients with suspicion of malignancy of Lymphoepithelial Carcinoma of the parotid gland. We also recommend that adjuvant radiotherapy is performed no later than 6 weeks after resection, taking into account that lymphoepithelial carcinoma is a high-grade carcinoma. Neoadjuvant chemotherapy might be useful for patients with bulky nodal disease to prevent micrometastases due to high tumor burden.
Acknowledgments
Our study was supported by Dharmais National Cancer Center Hospital. We would like to thank the patient in this study and all staff in Research and Development Department Dharmais National Cancer Center Hospital.
Funding Statement
This study was funded by Dharmais National Cancer Center Hospital, Indonesia.
Conflict of Interest
All authors have no potential conflict of interest.
Ethics Approval and Consent to Participate
This study was approved by Ethical Committee at Dharmais Hospital-National Cancer Center, Indonesia (Number of Ethical Clearance: 035/KEPK/II/2022).
References
- Lymphoepithelial carcinoma of the salivary glands Kim YJ , Hong HS , Jeong SH , Lee EH , Jung MJ . Medicine.2017;96(7). CrossRef
- Major and minor salivary gland tumors Guzzo M, Locati LD , Prott FJ , Gatta G, McGurk M, Licitra L. Critical Reviews in Oncology/Hematology.2010;74(2). CrossRef
- Incidence of carcinoma of the major salivary glands according to the WHO classification, 1992 to 2006: a population-based study in the United States Boukheris H, Curtis RE , Land CE , Dores GM . Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology.2009;18(11). CrossRef
- Survival in oral cavity minor salivary gland carcinoma Kakarala K, Bhattacharyya N. Otolaryngology--Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery.2010;143(1). CrossRef
- Lymphoepithelial carcinoma in parotid gland related to EBV infection: A case report Maeda H, Yamashiro T, Yamashita Y, Hirakawa H, Agena S, Uehara T, et al . Auris Nasus Larynx.2018;45(1):170-174.
- Lymphoepithelial carcinoma: a case of a rare parotid gland tumor Tang CG , Schmidtknecht TM , Tang GY , Schloegel LJ , Rasgon B. The Permanente Journal.2012;16(3).
- Lymphoepithelial carcinoma of the major salivary glands: Predictors of survival in a non-endemic region Zhan KY , Nicolli EA , Khaja SF , Day TA . Oral Oncology.2016;52. CrossRef
- Primary lymphoepithelial carcinoma of the intraoral minor salivary gland: A case report Zeng M, Li S, Fu J, Wu H, Gao Y. Oncology Letters.2015;9(2). CrossRef
- Neoplasms of the salivary glands: Lymphoepithelial Carcinoma. In: Atlas of Head and Neck Pathology. 3rd ed Wenig BM , Heffess C. Philadelphia: Elsevier Health Sciences.2015.
- CT features and pathologic characteristics of lymphoepithelial carcinoma of salivary glands Zhang G, Tang J, Pan Y, Zhuang Q, Wu C. International Journal of Clinical and Experimental Pathology.2014;7(3).
- Management of a Rare Lymphoepithelial Carcinoma of the Submandibular Gland in Elderly Sairin ME , Yahya N, Kuan CY , Yunus MRM , Abdullah MK . Indian Journal of Otolaryngology and Head and Neck Surgery: Official Publication of the Association of Otolaryngologists of India.2019;71(Suppl 1). CrossRef
- Lymphoepithelial carcinoma of the parotid glands and its relationship with benign lymphoepithelial lesions Schneider M, Rizzardi C. Archives of Pathology & Laboratory Medicine.2008;132(2). CrossRef
- Clinicopathologic study of 1176 salivary gland tumors in a Chinese population: experience of one cancer center 1997-2007 Wang Y, Zhu Y, Chen T, Wang Y, Sun G, Zhang L, Huang C, Wang Z, Shen Q, Li D, Wu Y, Ji Q. Acta Oto-Laryngologica.2012;132(8). CrossRef
- Case Report Lymphoepithelioma-Like Carcinoma of the Salivary Gland: Is Radiotherapy Alone Adequate? Hindawi Publishing Corporation Case Reports in Otolaryngology Volume 2011, Article ID 618650, 4 page Orit Kaidar-Person , Abraham Kuten , Salem Billan . 2011. CrossRef
- A clinical analysis of 37 cases with lymphoepithelial carcinoma of the major salivary gland treated by surgical resection and postoperative radiotherapy: a single institution study Li F, Zhu G, Wang Y, Wang Y, Chen T, Ji Q. Medical Oncology (Northwood, London, England).2014;31(5). CrossRef
- Undifferentiated nasopharyngeal cancer (UCNT): current diagnostic and therapeutic aspects Altun M., Fandi A., Dupuis O., Cvitkovic E., Krajina Z., Eschwege F.. International Journal of Radiation Oncology, Biology, Physics.1995;32(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times