The Impact of Colon Cancer Sites on Survival Rates after Curative Resection and Adjuvant Chemotherapy: A SingleCenter Study
Download
Abstract
Background: Most recent studies indicate that right-sided colon cancer is associated with a significantly higher mortality rate. Multivariate analyses showed that the patient’s age, sex, mode of presentation, co-morbidity, and the stage had significantly influenced their survival. Although the primary tumor location has an impact on the overall survival in metastatic settings, the laterality of early-stage colon cancer might also affect the disease-free survival and determine the duration of adjuvant chemotherapy for each side. This study aimed to compare overall survival and disease-free survival between left-sided and right-sided high-risk stage II and stage III colon cancer in patients from a single institute.
Methods: This retrospective cohort study was conducted between January 2004 and December 2017. Data on 153 patients who underwent curative resection and adjuvant chemotherapy for colon cancer were retrieved from an existing database.
Results: We found that the five-year disease-free survival rates were 63.20% for left-sided colon cancer and 51.11% for right-sided colon cancer (P-value < 0.05). The five-year overall survival rates were 66.98% for left-sided colon cancer and 57.77% for right-sided colon cancer (P-value 0.063). The right-sided primary tumor location was associated with a significantly higher mortality rate (HR: 2.28; 95%CI 1.38–5.8; P-value: 0.004).
Conclusion: The results of this study confirmed that patients with high-risk stage II and stage III colon cancer who had right-sided tumors were significantly more likely to have decreased disease-free survival and overall survival. Further prospective studies should focus on tumor genetics and proper durations of adjuvant chemotherapy to maximize the benefit of treatment with acceptable toxicity.
Introduction
Colorectal cancer is common cancer in the Asia population. Factors that affect the survival rate [1] include the patient’s age, the presence of comorbidities, tumor grading, and the timing of the onset of symptoms. We currently have evidence that the laterality of colorectal cancer might affect the disease-free survival rate and overall survival rate [2]. This tendency can be explained by the embryology mid-gut and hind-gut [3]. It was first observed and reported in the 1980s [4]. Therefore, it is interesting to note that the laterality of colon cancer may influence survival outcomes [5-7]. This study aimed to assess the impact of the laterality of colon cancer on survival outcomes in early-stage settings.
Materials and Methods
Eligible cases were obtained by searching the ICD 10 diagnostic code C180-C19 for colon cancer in a retrospective medical database between January 1, 2004, and December 31, 2017, in the Police General Hospital. We included patients aged more than 18 years old with stage II high-risk and stage III colon cancer, as classified using the current AJCC 8th staging system, who had completed adjuvant chemotherapy [8]. Patients with either rectal cancer or colon cancer as a second primary cancer and those who visited the hospital irregularly were excluded from the study. All patients were followed up, for at least five years, until December 31, 2021.
Sample size
We estimated the sample size using the equation for cohort studies with binary outcomes.
The prevalence of colon cancer from a previous study [2] and the five-year recurrence rates for right-sided colon cancer (61.1%) and left-sided colon cancer (81.9%) were used in the sample size calculation (P < 0.05). Thus, the calculated sample size was 146 cases.
Descriptions of study variables
The disease-free survival was defined as the time-lapse between primary surgery and the documented date of disease recurrence as corroborated by radiological report confirmations. The overall survival was defined as the time-lapse between primary treatment and death of any cause. Right-sided colon cancer was defined as cancer affecting the cecum, ascending colon, and transverse colon. Left-sided colon cancer was defined as cancer affecting the splenic flexure, descending colon, and sigmoid colon. The primary endpoint of this study was to compare the disease-free survival (DFS) between the sides of stage II and stage III colon cancer. The difference in the overall survival (OS) was a secondary endpoint in this study .
Statistical analyses
The Shapiro-Walk test was used to check the normality of data distribution. Continuous variables were presented as mean values and standard deviations (for normally distributed data) or median values and interquartile ranges (IQRs) for variables with skewed data distributions. Comparisons between two groups were performed with either the Chi-square test or Fisher’s Exact test. The DFS and OS were determined via the Kaplan- Meier curve. The Cox proportional hazard regression model and the Log-rank test were used to perform estimations and between-group comparisons. Univariate and multivariate analyses were also performed using Cox’s proportional hazard regression. All statistical analyses were performed using R. The research protocol was approved by the Institutional Review Board of the Police General Hospital. This protocol was registered in the Thai clinical trials registry (TCTR20161219003).
Results
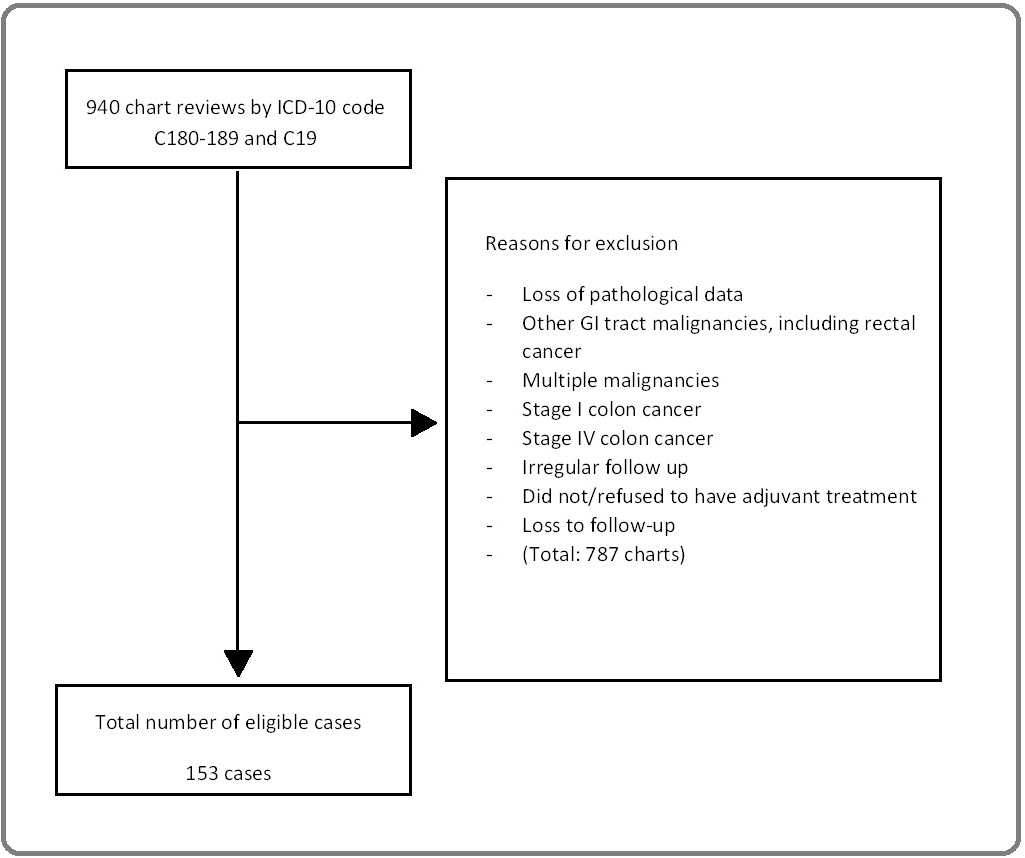
Nine hundred and forty cases were included. After cleaning the data, there were 153 eligible cases (Figure 1) with a median follow-up duration of 75.4 months.
Figure 1. The Consort Diagram.
The baseline patient characteristics are shown in Table 1.
| Characteristics | Number of patients | Left side colon | Right side colon |
| Patients | 153 | 108 | 45 |
| Age, Years; mean ± SD | 62.21 ± 10.90 | 61.44 ± 11.11 | 64.07 ± 10.27 |
| Min-Max | 35–86 | 35–86 | 42–66 |
| <65 | 91 | 68 | 23 |
| ≥65 | 62 | 40 | 22 |
| Sex | |||
| Male (%) | 95 (62.1) | 65 (60.2) | 30 (66.7) |
| Female (%) | 58 (37.9) | 43 (39.8) | 15 (33.3) |
| Nodal status | |||
| N0-1 (%) | 104 (68) | 73 (67.6)) | 31(68.9) |
| N0 2–3 (%) | 49 (32) | 35 (32.4) | 14 (31.1) |
| Colon cancer staging | |||
| Stage 2 (%) | 58 (37.9) | 42 (39.9) | 16 (35.6) |
| Stage 3 (%) | 95 (62.1) | 66 (61.1) | 29 (64.4) |
| Grading of tumor | |||
| Well differentiated (%) | 83 (54.2) | 59 (54.6) | 24 (53.3) |
| Moderate differentiated (%) | 65 (42.5) | 47 (43.5) | 18 (40.0 |
| Poor differentiated (%) | 5 (3.3) | 2 (1.9) | 3 (6.7) |
| Received Oxaliplatin (%) | 87 (56.9) | 59 (54.6) | 28 (62.2) |
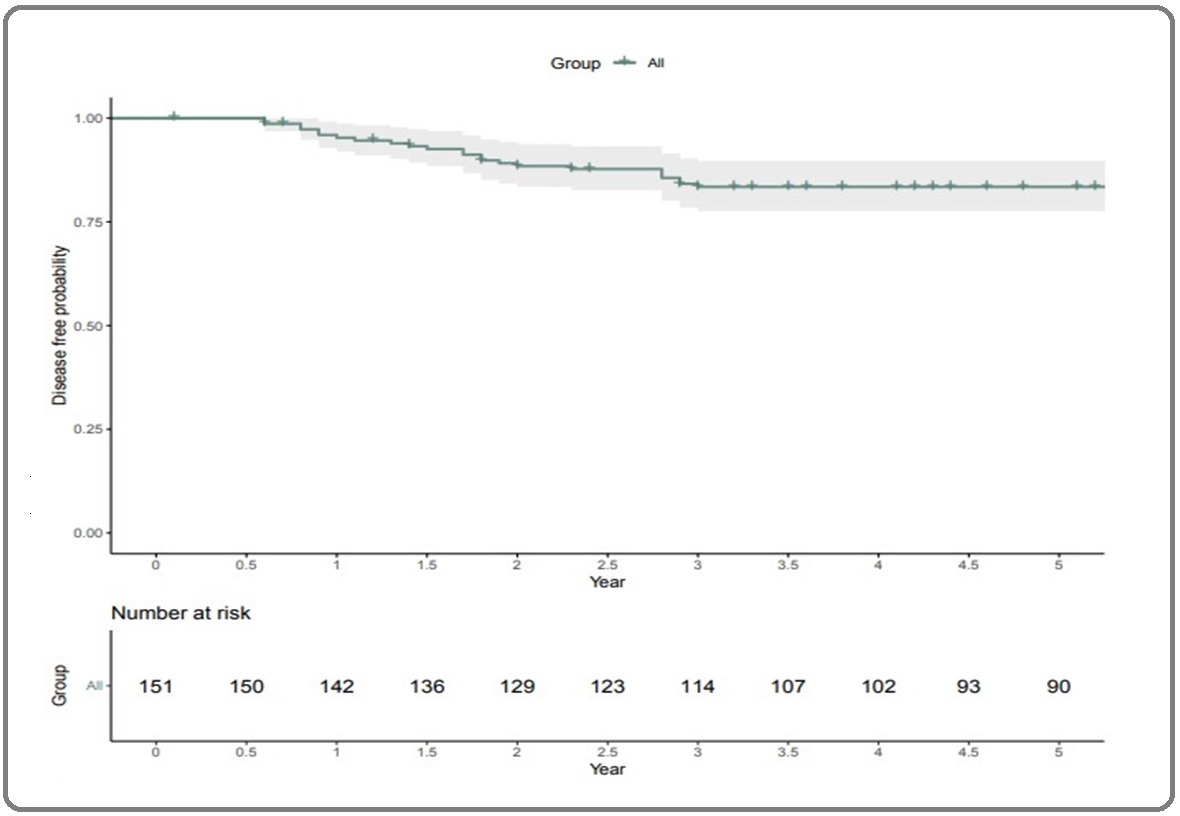
The mean age was 61.4 years in the left-sided colon cancer group and 64.7 years in the right-sided colon cancer group. Well differentiated morphologies were found predominantly in left-sided colon cancer (54.6%), and most cases (approximately 62.1%) were stage III colon cancer. The five-year DFS rate in this study was 59.6% (Figure 2).
Figure 2. Disease-free Survival of Stage II and Stage III Colon Cancer.
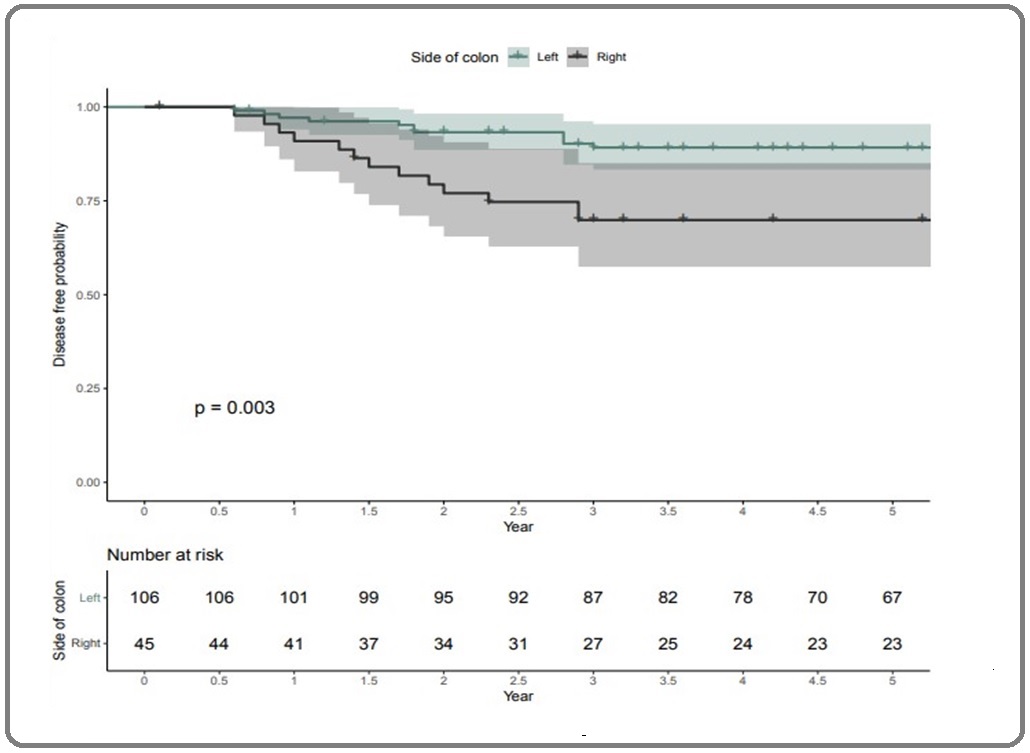
There was a significant difference in the five-year DFS rates between the left-sided and right-sided colon cancer groups (63.2% vs. 51.11%, respectively; p = 0.003, Figure 3).
Figure 3. Comparing the Disease-free Survival of Left-sided Colon Cancer and Right-sided Colon Cancer.
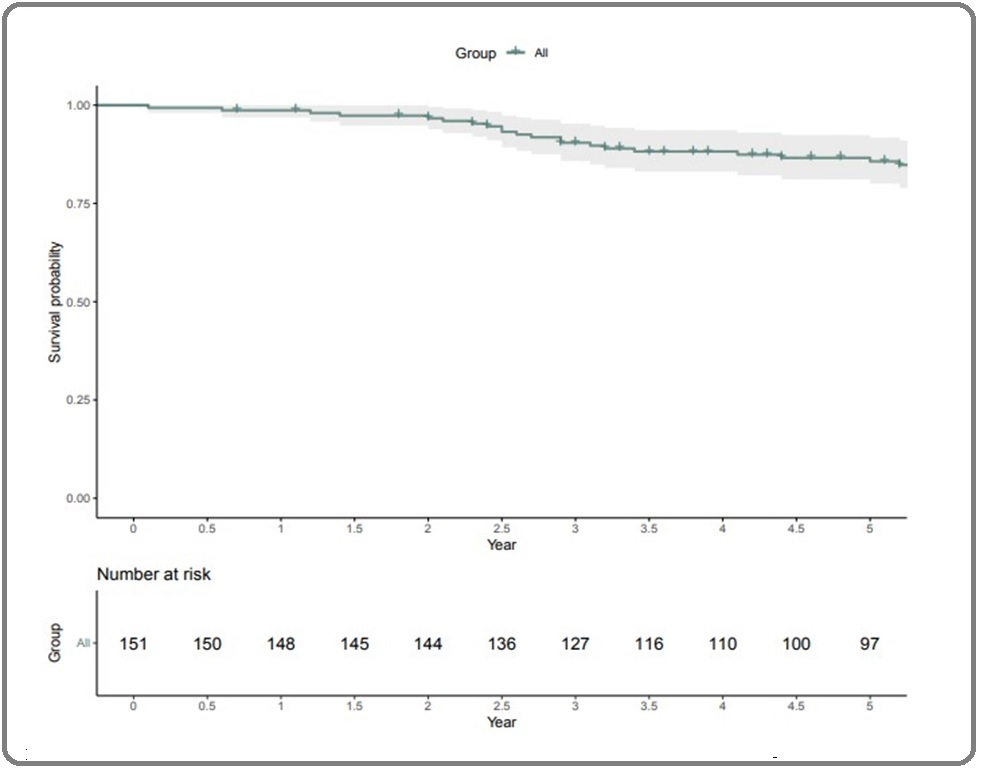
The five-year OS rate in this study was 64.23% (Figure 4).
Figure 4. Overall Survival of Stage II and Stage III Colon Cancer.
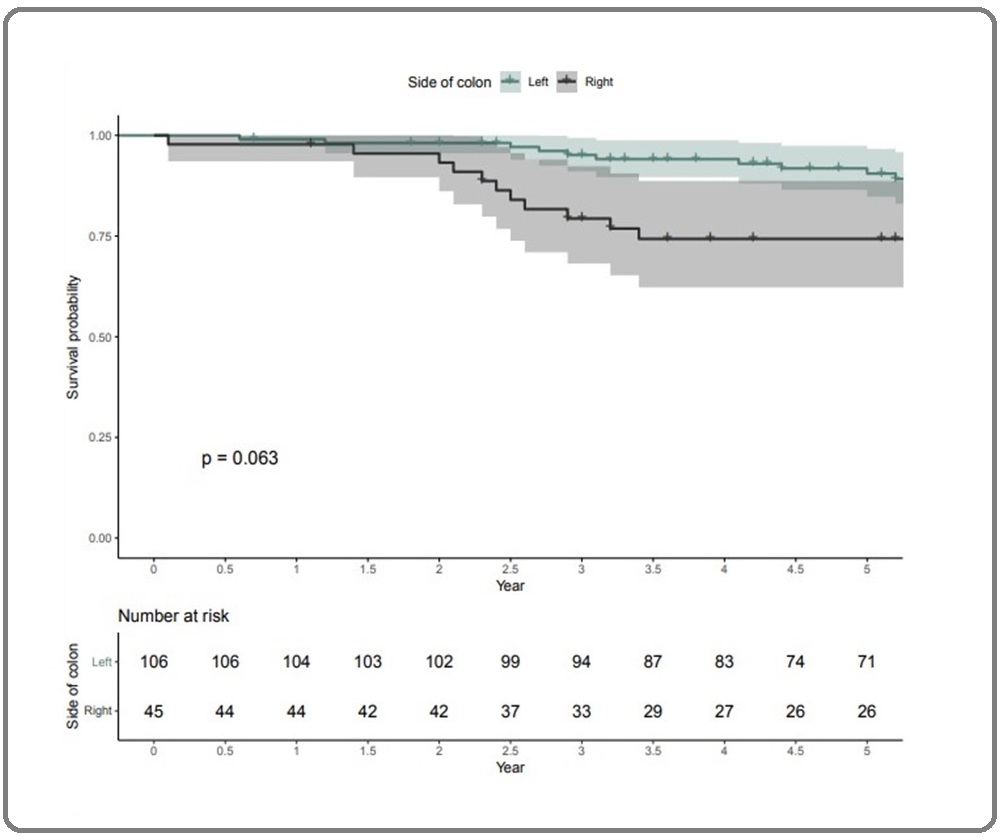
The five-year OS rate in left-sided colon cancer (66.98%) was higher than that in right-sided colon cancer (57.7%; p = 0.063, Figure 5).
Figure 5. Comparing the Overall Survival of Left-sided Colon Cancer and Right-sided Colon Cancer.
Through the adjusted Cox proportional hazard ratio of high-risk stage II and stage III colon cancer from multivariable analysis, we found that right-sided colon cancer had shorter survival than left-sided colon cancer (HR 2.28; p-value = 0.004: 95%CI 1.38–5.8, Table 2).
| Factors | Coefficient | HR (95%CI) | p-value | Adjusted HR (95%CI) | p-value |
| Age | 0.021 | 1 (0.987–1.06) | 0.221 | 1.484 (0.6691–3.293) | 0.331 |
| Age > 65 years | 0.17 | 1.2 (0.578–2.45) | 0.637 | ||
| Male | 0.53 | 1.7 (0.775–3.7) | 0.186 | ||
| Colon cancer stage III | 0.8 | 2.2 (0.957–5.2) | 0.063 | 1.777 (0.6813–4.635) | 0.239 |
| N stage II–III | 0.68 | 2 (0.962–4.05) | 0.063 | 1.570 (0.6869–3.590) | 0.285 |
| Right side colon cancer | 1 | 2.8 (1.38–5.8) | 0.004 | 2.875 (1.3965–5.920) | 0.004 |
Discussion
Colon cancer is one of the top five most common types of cancer worldwide. The hypothesis of different embryological origins for the different sides of colon cancer is displayed in molecular and tumor genetics and might affect the survival outcomes. It was observed initially in metastatic settings from previous studies. Studies on advanced colorectal cancer revealed that left-sided colon cancer has better median survival than right-sided colon cancer with regorafenib treatment, even based on biomarkers with PFS durations of 2.6 months and 1.9 months, respectively (p = 0.04) [9]. Another study showed some differences in tumor genetic markers such as the BRAF mutation and microsatellite instability (MSI) of right-sided and left-sided colon cancer also affect the survival outcomes [10]; however, the median survival of advanced right-sided colon cancer was still lower than that of advanced left-sided colon cancer (13.2 vs. 20 months). Regarding the frontline treatment of the KRAS mutation in advanced colon cancer [11], it was shown that cetuximab treatment for KRAS wild-type, left-sided colon cancer was superior in terms of OS (35.8 months vs. 14.4 months; p = 0.031); however, no significant difference was found in the OS when treated with bevacizumab. However, there were two studies that showed no significant difference in the prognosis and OS outcome between right-sided and left-sided colon cancer [12, 13]. Recent population-based studies conducted in the Norwegian population that included all stages of colon cancer showed increasing survival trends with left-sided colon cancer over the past four decades [14]. In the adjuvant setting, a meta-analysis by Petrelli et al. that included colon cancer of different stages (stages I, II, and III) confirmed that the left-sided location of tumors was associated with better survival outcomes (HR 0.84; 95% CI, 0.79–0.89; p < 0.001) [15]. Several studies confirmed that the five-year OS of right-sided colon cancer after curative surgery is lower than of left-sided colon cancer (82.1% vs. 88.7%; p < 0.05) [2]. In Japan, a cancer registry-based study also showed that the anatomical side of the colon could be a prognostic factor, especially in advanced-stage colon cancer [16]. Our study also showed that patients with right-sided colon cancer had an average age of 64.07 years while the average age of patients with left-sided colon cancer was 61.44 years. Other previous studies showed that right-sided colon cancer has lower survival rates than left-sided colon cancer [17]. Regarding adjuvant chemotherapy, the combination of oxaliplatin and 5-fluorouracil (5FU), including oral 5FU derivatives such as capecitabine, is a standard adjuvant treatment. The MSI test becomes important in adjuvant settings, especially in stage II colon cancer [18]. Previous studies revealed that MSI-high, especially in stage II colon cancer, 5FU-based regimens may add only a little benefit to the treatment [19-21]; however, some patients with stage III colon cancer with MSI-high have better prognoses than microsatellite stability patients. Unlike fluorouracil, oxaliplatin does not affect the MSI status [18, 22]. Our findings confirmed that early-stage left-sided colon cancer has a five-year OS rate of 66.98% while right-sided colon cancer had a rate of 57.77%. We also found that left-sided colon cancer responds better to adjuvant chemotherapy than right-sided colon cancer. A poorly-differentiated morphology was also found in right-sided colon cancer more than in left-sided colon cancer in our study. Also, in line with the findings of other studies, the incidence of left-sided colon cancer is higher than that of right-sided colon cancer. However, our study had certain limitations. First, there was a paucity of data on tumor genetic mutations such as MSI and KRAS because genetic testing is not routine in our clinical practice. Second, this study was a retrospective, single-center study, and the data collected were based on medical records. Some important information was incomplete, which resulted in a decrease in the number of eligible cases and the amount of data that could be analyzed. Nevertheless, our results were still consistent with those of previous studies.
In conclusion, our study findings confirmed that left-sided colon cancer had a better prognosis in the early-stage. Prospective studies involving multicenter data and tumor genetic exploration for each side of the colon should be performed in the future. Future studies including optimal durations of oxaliplatin-based chemotherapy should be conducted based on the laterality of colon cancer and based on tumor genetic information. This will bring more precision to personalized treatment in the future.
References
- Possible better long-term survival in left versus right-sided colon cancer - a systematic review Hansen IO , Jess P. Danish Medical Journal.2012;59(6).
- Comparison of oncological outcomes of right-sided colon cancer versus left-sided colon cancer after curative resection: Which side is better outcome? Lim DR , Kuk JK , Kim T, Shin EJ . Medicine.2017;96(42). CrossRef
- Difference between right-sided and left-sided colorectal cancers: from embryology to molecular subtype Yang SY , Cho MS , Kim NK . Expert Review of Anticancer Therapy.2018;18(4). CrossRef
- Trends in right and left-sided colon cancer Beart R. W., Melton L. J., Maruta M., Dockerty M. B., Frydenberg H. B., O'Fallon W. M.. Diseases of the Colon and Rectum.1983;26(6). CrossRef
- Colon Cancer, Version 1.2017, NCCN Clinical Practice Guidelines in Oncology Benson AB , Venook AP , Cederquist L, Chan E, Chen Y, Cooper HS H, Deming D, et al . Journal of the National Comprehensive Cancer Network: JNCCN.2017;15(3). CrossRef
- Primary tumor location as a prognostic factor in metastatic colorectal cancer Loupakis F, Yang D, Yau L, Feng S, Cremolini C, Zhang W, Maus MKH , et al . Journal of the National Cancer Institute.2015;107(3). CrossRef
- Does the primary site of colorectal cancer impact outcomes for patients with metastatic disease? Price TJ , Beeke C, Ullah S, Padbury R, Maddern G, Roder D, Townsend AR , et al . Cancer.2015;121(6). CrossRef
- The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging Amin MB , Greene FL , Edge SB , Compton CC , Gershenwald JE , Brookland RK , Meyer L, et al . CA: a cancer journal for clinicians.2017;67(2). CrossRef
- The Impact of Primary Tumor Sidedness on the Effect of Regorafenib in Refractory Metastatic Colorectal Cancer Yoon SE , Lee SJ , Lee J, Park SH , Park JO , Lim HY , Kang WK , Park YS , Kim ST . Journal of Cancer.2019;10(7). CrossRef
- Right Sided Colon Cancer as a Distinct Histopathological Subtype with Reduced Prognosis Nitsche U, Stögbauer F, Späth C, Haller B, Wilhelm D, Friess H, Bader FG . Digestive Surgery.2016;33(2). CrossRef
- Primary tumor location is an important predictive factor for wild-type KRAS metastatic colon cancer treated with cetuximab as front-line bio-therapy Lu H, Lin J, Chen W, Jiang J, Yang S, Lan Y, Lin Chun-Chi, Chang S, Teng H. Asia-Pacific Journal of Clinical Oncology.2016;12(3). CrossRef
- Clinicopathological characteristics and prognostic impact of colorectal cancers with NRAS mutations Ogura T, Kakuta M, Yatsuoka T, Nishimura Y, Sakamoto H, Yamaguchi K, Tanabe M, Tanaka Y, Akagi K. Oncology Reports.2014;32(1). CrossRef
- High miR-21 expression from FFPE tissues is associated with poor survival and response to adjuvant chemotherapy in colon cancer Oue N, Anami K, Schetter AJ , Moehler M, Okayama H, Khan MA , Bowman ED , et al . International Journal of Cancer.2014;134(8). CrossRef
- Survival Trends of Right- and Left-Sided Colon Cancer across Four Decades: A Norwegian Population-Based Study Hamfjord J, Myklebust TA , Larsen IK , Kure EH , Glimelius B, Guren TK , Tveit KM , Guren MG . Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology.2022;31(2). CrossRef
- Prognostic Survival Associated With Left-Sided vs Right-Sided Colon Cancer: A Systematic Review and Meta-analysis Petrelli F, Tomasello G, Borgonovo K, Ghidini M, Turati L, Dallera P, Passalacqua R, Sgroi G, Barni S. JAMA oncology.2017;3(2). CrossRef
- Impact of Tumor Location and Variables Associated With Overall Survival in Patients With Colorectal Cancer: A Mayo Clinic Colon and Rectal Cancer Registry Study Wang CB , Shahjehan F, Merchea A, Li Z, Bekaii-Saab TS , Grothey A, Colibaseanu DT , Kasi PM . Frontiers in Oncology.2019;9. CrossRef
- Clinico-pathological and oncological differences between right and left-sided colon cancer (stages I-III): analysis of 950 cases Cienfuegos JA , Baixauli J, Arredondo J, Pastor C, Martínez Ortega P, Zozaya G, Martí-Cruchaga P, Hernández Lizoáin JL J. Revista Espanola De Enfermedades Digestivas: Organo Oficial De La Sociedad Espanola De Patologia Digestiva.2018;110(3). CrossRef
- Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer Sargent DJ , Marsoni S, Monges G, Thibodeau SN , Labianca R, Hamilton SR , French AJ , et al . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2010;28(20). CrossRef
- Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer Ribic CM , Sargent DJ , Moore MJ , Thibodeau SN , French AJ , Goldberg RM , Hamilton SR , Laurent-Puig P, Gryfe R, Shepherd LE , Tu D, Redston M, Gallinger S. The New England Journal of Medicine.2003;349(3). CrossRef
- Mismatch Repair and Colon Cancer: Mechanisms and Therapies Explored Li SKH , Martin A. Trends in Molecular Medicine.2016;22(4). CrossRef
- The evolving role of microsatellite instability in colorectal cancer: A review Gelsomino F, Barbolini M, Spallanzani A, Pugliese G, Cascinu S. Cancer Treatment Reviews.2016;51. CrossRef
- Efficacy of Adjuvant Chemotherapy in Colon Cancer With Microsatellite Instability: A Large Multicenter AGEO Study Tougeron D, Mouillet G, Trouilloud I, Lecomte T, Coriat R, Aparicio T, Des Guetz G, et al . Journal of the National Cancer Institute.2016;108(7). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times