A Case Series of Partial Cystectomy without Frozen Section
Download
Abstract
Background: Bladder cancer is a common type of urinary system cancer in the world with high morbidity and mortality if not managed optimally. Currently, partial cystectomy has experienced a resurgence as a less morbid and oncologically effective treatment. Here, we appropriately diagnosed and surgically treated 5 patients with partial cystectomy without frozen section and reviewed the outcome of this procedure.
Case presentation: The diagnosis was made based on the history of illness, physical examination, CT-Scan, and confirmed by histopathological examination. A partial cystectomy was performed in all cases, which include laparoscopic partial cystectomy. Based on histological examination, we found that 4 cases in this study were adenocarcinoma bladder and 1 case was urothelial carcinoma cells with sarcomatoid variant. Our surgical technique started with doing a cystoscopy first. We performed excision of the tumor with lateral margin 1cm around the tumor. After resection of the tumor, we closed the bladder and evaluated the capacity of the bladder, which was 200cc minimal capacity. Then we closed the bladder with the double layer technique and closed the muscle, fascia, and skin, respectively. Follow-up was performed 6 and 12 months after surgery to observe progression or recurrence of the tumor. There was no postoperative complication in our case. All of our cases had no complaints and no sign of progression, recurrence, and metastatic sign.
Conclusion: A frozen section has not been proven to be mandatory in partial cystectomy and the results had no significant effect in surgical margins. A Partial cystectomy had a good result and improved the quality of patient life with preserved the bladder function.
Introduction
Bladder cancer is a common type of urinary system cancer in the world and estimated that every year there are more than 500,000 new cases [1,2]. As a complex disease, bladder cancer has high morbidity and mortality if not managed optimally [1]. This cancer is treated based on the pathological degree of disease and on the subsequent staging according to tumor lymph node metastasis. Non-muscle invasive bladder cancer (NMIBC) is most commonly treated with transurethral resection of bladder tumor (TURBT) and followed by intravesical bacille Calmette-Guérin or intravesical chemotherapy. When bladder tumors invade the muscles layer, it usually treated with radical cystectomy and prolonged lymphadenectomy, followed by cisplatin-based neoadjuvant chemotherapy because of higher rates of progression and recurrence [3]. Currently, partial cystectomy has experienced a resurgence as a less morbid and oncologically effective treatment.
Over the past decade, some of the literature has argued that partial cystectomy represents a viable alternative to radical cystectomy and deserves discussion among the standard of care options for select patients [4]. Here, we appropriately diagnosed and surgically treated 5 patients with partial cystectomy without frozen section and reviewed the outcome of this procedure.
Materials and Methods
The study was conducted on five cases of bladder tumors that required surgical operation of tumor at Hasan Sadikin General Hospital – Indonesia, a tertiary academic hospital. Patient characteristics and follow-up can be seen in Table 1.
| Result | |
| Age (Year) | 46.5 (24-62) |
| Gender | |
| Male | 3 (60%) |
| Female | 2 (40%) |
| Tumor size | |
| <3cm | 0 |
| ≥3 cm | 5 (100%) |
| Histology | |
| Urothelial carcinoma | 1 (20%) |
| Adenocarcinoma | 3 (60%) |
| Other | 1 (20%) |
| T Stage | |
| Non-muscle invasive | 1 (20%) |
| Muscle invasive | 4 (80%) |
| Surgical margin | |
| Positive | 1 (20%) |
| Negative | 4 (80%) |
| Lymph node involvement | |
| Yes | 1 (20%) |
| No | 4 (80%) |
| Hydronephrosis | |
| Yes | 0 (0%) |
| No | 5 (100%) |
The diagnosis was made based on the history of illness, physical examination, CT-Scan, and confirmed by histopathological examination (Table 2 and Figure 1).
| No | Patient | Symptoms | Imaging (location & size) | Surgical | Surgical Margin | Histopathology | Follow Up (Symptoms & USG) | Survival |
| 1 | Male 45 years old ECOG 0 | Hematuria | Anterior wall with size 7x6x5cm | Partial cystectomy + Pelvic lymph node dissection | Positive | Urothelial carcinoma pT3bN2M0 | Adjuvant chemotherapy 4 cycles (Gemcitabine & Cisplatine) No hematuria No lesion on USG every 6 months | > 5 years |
| 2 | Female 55 years old ECOG 0 | Hematuria | Anterior wall with size 7x6x6cm | Partial cystectomy + Pelvic lymph node dissection | Negative | Adenocarcinoma bladder pT3bN0M0 | No hematuria No lesion on USG every 6 months | >2 year |
| 3 | Male 24 years old ECOG 0 | Mucosuria | Anterior bladder wall and patent ductal urachal | Partial cystectomy + Excision of patent ductus urachus | Negative | Fibromuscular tissue on patent ductal urachal | No hematuria No lesion on USG every 6 months | >2 year |
| 4 | Male 62 years old ECOG 0 | Hematuria | Anterior bladder wall with size 6x5x4cm | Partial cystectomy + Pelvic lymph node dissection | Negative | Adenocarcinoma bladder pT3bN0M0 | No hematuria No lesion on USG every 6 months | >1 year |
| 5 | Female 48 years old ECOG 0 | Hematuria | Anterior bladder wall with size 7x7x5cm | Laparoscopic partial cystectomy + Pelvic lymph node dissection | Negative | Adenocarcinoma bladder pT2N0M0 | No hematuria No lesion on USG every 6 months | >1 year |
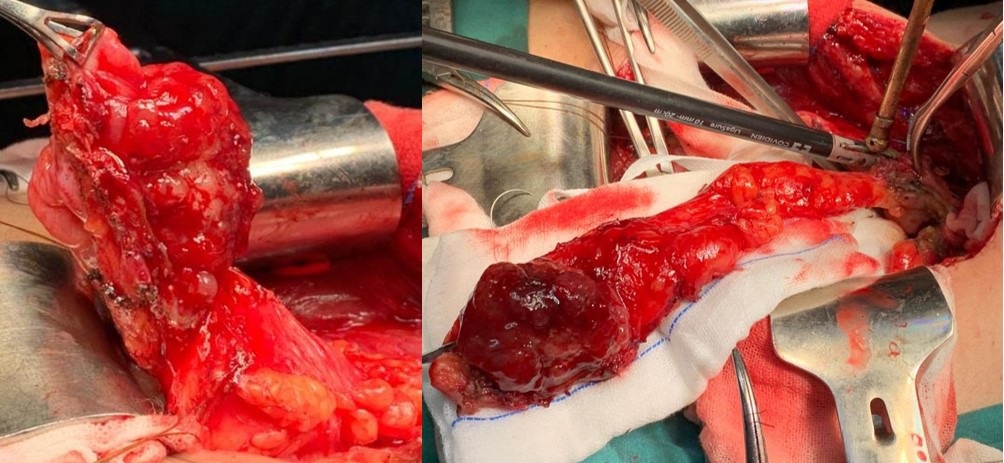
Figure 1. Open Approach. Wide Surgical Excision of the Portion of Bladder.
A partial cystectomy was performed in all cases, which include laparoscopic partial cystectomy. Based on histological examination, we found that 4 cases in this study were adenocarcinoma bladder and 1 case was urothelial carcinoma cells with sarcomatoid variant. Follow-up was performed 6 and 12 months after surgery to observe progression or recurrence of the tumor. There was no postoperative complication in our case. All of our cases had no complaints and no sign of progression, recurrence, and metastatic sign.
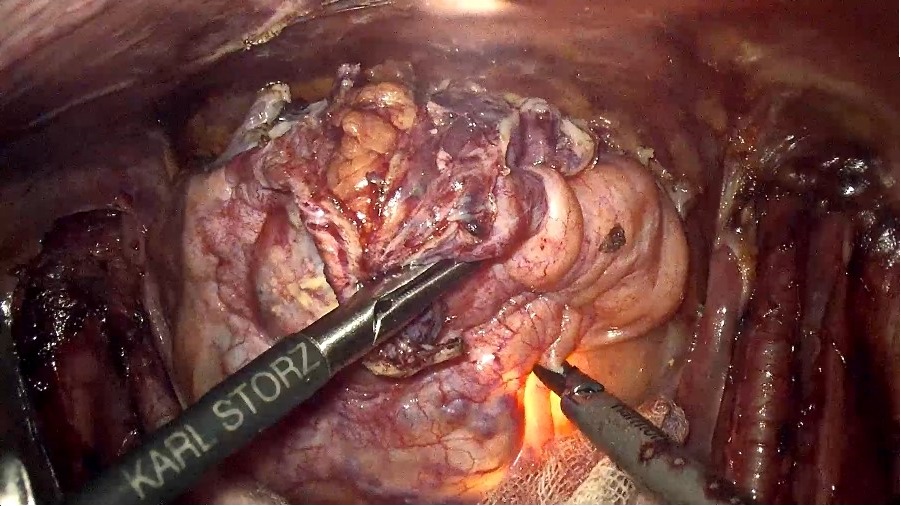
Our surgical technique started with doing a cystoscopy first. We evaluated all of the bladder regions, then assessed the mass inside the bladder. The tumor was assessed for size with a cutting loop, then tattooed around the tumor was done in a circle with a collin knife. Next, we performed midline laparotomy incision, dissection fascia, muscle, and peritoneum upward. We assessed the lymph node around the bladder and performed pelvic lymph node dissection. Then, we opened the bladder in the area that not infiltrated with the tumor. We performed excision of the tumor with lateral margin 1cm around the tumor (Figure 1 and 2).
Figure 2. Laparoscopic Approach. Noted the Light from Cystoscopy as a Guide Mass Excision.
After resection of the tumor, we closured the bladder and evaluated the capacity of the bladder, which was 200cc minimal capacity. Then we closed the bladder with the double layer technique and closed the muscle, fascia, and skin, respectively.
Case Description
Case 1 A 45-years-old male patient presented with a chief complaint of red-colored urine. Physical examination was normal and ECOG score performance status was 0. We found a non-homogenous mass in the bladder at the anterior bladder wall with size 6x6x5 cm from abdominal and pelvic CT Scan, without lymph nodes, urethra, and prostate involvement. We performed a partial cystectomy and pelvic lymph node dissection. The macroscopic finding was a 6x4cm solid mass. The histopathological result was urothelial carcinoma pT3bN2MO with involvement left external iliac lymph node. The patient underwent adjuvant chemotherapy with full-cycle gemcitabine. On the 3 and 6 months follow-up, abdominal CT scan, chest X-ray, and lab results were within normal limits. During 12 months follow-up, the patient reported no complaint, and imaging showed no recurrence until 5 years follow-up.
Case 2 A 55-years-old female patient presented with a chief complaint of red-colored urine. Physical examination was normal with ECOG score performance status was 0. An abdominal CT scan showed an inhomogeneous lesion in the anterior bladder wall with size 7x5x4cm, without the involvement of lymph nodes, urethra, and prostate. We performed a partial cystectomy and pelvic lymph node dissection. The macroscopic finding was a 7x4cm solid mass. The histopathological result was adenocarcinoma pT3Bn0M0 with a negative surgical margin and no involvement of lymph nodes. During 12 months follow-up, the patient reported no complaint, and imaging showed no recurrence sign.
Case 3 A 24-years-old male patient presented with a chief complaint of mucosuria. The patient had a history of urine coming out from the umbilical 2 times. Physical examination showed a normal form of abdomen and umbilical. Patient ECOG performance status was 0. An abdominal CT scan showed a single mass in the anterior bladder wall that connected to the umbilical. We performed a partial cystectomy, excision of patent ductus urachus, and pelvic lymph node dissection. The histopathological result was fibromuscular tissue and normal urothelium without malignancy signs. The surgical margin was negative. Follow-up was performed with results the patient had no complaints and recurrence during 12 months after surgery.
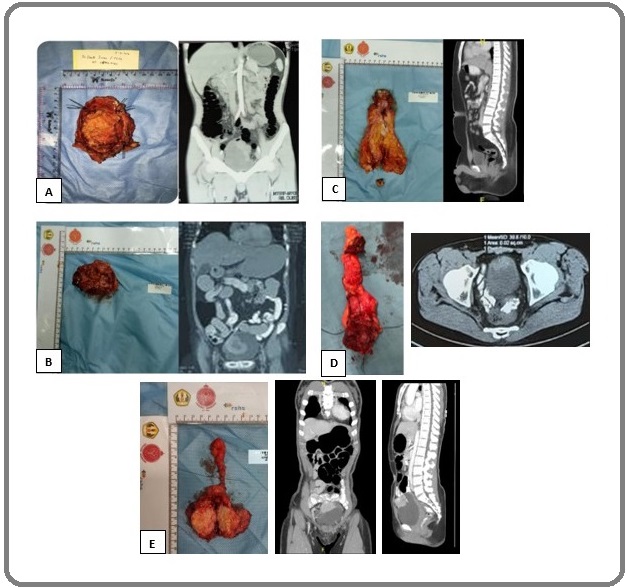
Case 4 A 62-years-old patient presented with a chief complaint of red-colored urine. Physical examination was normal with ECOG performance status was 0. The abdominal CT Scan with contrast revealed a bladder tumor at the anterior wall of the bladder with a size 6x5x4cm. We performed a partial cystectomy and pelvic lymph node dissection. The histopathological result was adenocarcinoma pT3bN0M0 with a negative surgical margin and no involvement of lymph nodes. During 6 months follow-up, the patient reported no complaint, and imaging showed no recurrence sign. Case 5 A 48-years-old patient presented with a chief complaint of red-colored urine. Physical examination was normal with ECOG performance status was 0. The abdominal CT Scan with contrast revealed a bladder tumor at the anterior wall of the bladder with a size 7x7x5cm. We performed a laparoscopic partial cystectomy and pelvic lymph node dissection. The histopathological result was adenocarcinoma pT2N0M0 with a negative surgical margin and no involvement of lymph nodes. During 6 months follow-up, the patient reported no complaint, and imaging showed no recurrence sign (Figure 3).
Figure 3. Computed Tomography (CT) and Post-Operative Bladder Mass. A. Case 1. Patient with Bladder tumor cT3bN2M0; B. Case 2. Patient with Bladder tumor cT3bN0M0; C. Case 3. Patient with Patent Urachus; D. Case 4. Patient with Bladder tumor cT3bN0M0. E. Case 5. Patient with Bladder tumor cT3bN0M0.
Discussion
Bladder cancer management depends on the pathologic extent of disease at the time that TURBT is performed and on subsequent staging according to the tumor-node- metastasis classification system. In addition, imaging such as CT or magnetic resonance imaging is often used to assess invasion beyond the bladder. Radical cystectomy with extended lymphadenectomy, preceded by cisplatin-based neoadjuvant chemotherapy are often used in bladder tumors that invade the muscle due to increased risk of progression and recurrence [3]. Radical cystectomy potentially impairs patients’ quality of life (QoL). Therefore, bladder-sparing strategies have been investigated to improve patients’ QoL without compromising oncological outcomes [5].
The purposes of bladder sparing are to maintain the optimal quality of life and preventing the risk of mortality and morbidity of radical cystectomy with preserving disease control. Reported 37 cases by Kassouf et al [6] had been showed partial cystectomy give sufficient cancer control in urothelial carcinoma of bladder patients [6]. Memorial Sloan-Kettering Cancer Center presented data of 58 patients for 6 years of period underwent partial cystectomy provide also good control outcome of the cancer in immensely selected patients [7]. The study conducted by Posielski et al. [8] proved that partial cystectomy had lower peri-operative mortality and overall survival comparable to radical cystectomy. Thus, selecting patients for partial cystectomy is essential. [8] Partial cystectomy could be done in certain patients include: A solitary tumor in an area amenable to resection, multiple tumors (<25% of the bladder surface) without involvement of the bladder neck or trigone, MSKCC stage 1 or 2 small tumors (<4 cm), situation in the upper half of the bladder, posterolateral wall of the bladder (can be resected with a reasonable margin ,1-2 cm, without the need for ureteral reimplantation, absence of multicentric disease in the upper urothelial tract, absence of metastatic disease at distant sites, absence of carcinoma in situ, the tumour-free margins of resection were confirmed by intraoperative frozen section examination, vigilant surveillance [5,9]. Certain conditions that contraindicated to partial cystectomy include: Cellular atypia in random biopsy specimens, prostatic invasion, bladder neck or trigonal invasion, presence of lymphovascular invasion in biopsy specimen, inability to achieve adequate surgical margins, prior radiation therapy, inadequate bladder volume following resection (<200cc), evidence of metastatic disease, poor preoperative performance status conveying high surgical risk.
Based on previous study, partial cystectomy is indicated to a solitary tumor in an area amenable to resection and absence of carcinoma in situ. For these patients, partial cystectomy represents a less morbid operation that maintains an intact bladder and voiding function, avoids the interposition of bowel into the urinary tract, and preserves sexual function [4]. Capitanio et al.[9] performed a matched analysis to compare radical and partial cystectomy and the results were partial cystectomy offered similar overall and cancer-specific survival [9]. Recurrence rate in 5 year of follow up post partial cystectomy are between 39% and 67% based on M.D. Anderson Cancer Center (2006) and Memorial Sloan-Kettering Cancer Center (2004) dat [4]. The case series conducted by Knoedler et al. [4] shown that partial cystectomy did not compromise outcomes when compared to radical cystectomy, some patients will nevertheless recur [4]. This is consistent in our series found that after 6 to 12 months follow up, all the patients had no complaint and recurrence although it does not rule out the possibility of recurrence in the future.
Intraoperative frozen section often routinely obtained for evaluation of microscopic presence at bladder margins. However, even frozen section contributes into risk reduction of cancer progression, two studies revealed that most patients showed negative frozen section results through additional tissue excision [10,11]. Sensitivity and specificity of frozen section of the urethral margins are 33-92% and 98–99% in radical cystectomy. Therefore, frozen section may cause a high rate of false positive in which potentially problematic. A study also presented that only 2.7% (three of 109) patients underwent frozen section during radical cystectomy has a positive result [12]. In partial cystectomy only a study reported in 7 patients underwent frozen section in partial cystectomy with negative results of surgical margins [13]. The effectivity of frozen section in partial cystectomy still needed more investigations. In our case, we performed frozen section without partial cystectomy with some considerations including only few data reported the frozen section in this surgical treatment with low sensitivity results, frozen section may lead to prolonged surgical duration, and our universal coverage of Indonesia also do not warranty for this kind of procedure.
In conclusion, partial cystectomy can be a treatment option in bladder cancer with proper patient selection, vigilant surveillance, and adjuvant administration should be strongly considered for patients with pathological evidence of extravesical expansion or pelvic lymph node metastases. A frozen section has not been proven to be mandatory in partial cystectomy and the results had no significant effect in surgical margins. A Partial cystectomy had a good result and improved the quality of patient life with preserved the bladder function.
Acknowledgements
The authors thank to every people contributed on the synthesis of this study.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
Declatation of interest
The author declare no conflict of interest.
Declaration of patient consent
We have obtained an appropriate patient consent form for his images and other clinical information to be reported in the article. The patient understands that his names and initials will not be published, and due efforts will be made to conceal his identity.
Consents and Ethics Approval
We have obtained written and oral consent from the patient to be included in this literature review and case report. Ethical approval was granted by our hospital ethical committee.
References
- Commentary : Bladder cancer Qi Y, Tang D. Curr Urol.2021;0(1):2021.
- Clinical Efficacy and Quality of Life Assessment of Partial Cystectomy and Plasmakinetic Transurethral Resection of Tumor in Bladder Cancer Patients Li Z, Wang D, Liu Z. Cancer Management and Research.2022;14. CrossRef
- Bladder Cancer: Diagnosis and Treatment Degeorge KC , Holt HR , Hodges SC . 2017.
- Organ-sparing surgery in urology: partial cystectomy Knoedler J, Frank I. Current Opinion in Urology.2015;25(2). CrossRef
- Selective bladder-sparing protocol consisting of induction low-dose chemoradiotherapy plus partial cystectomy with pelvic lymph node dissection against muscle-invasive bladder cancer: oncological outcomes of the initial 46 patients Koga F, Kihara K, Yoshida S, Yokoyama M, Saito K, Masuda H, Fujii Y, Kawakami S. BJU international.2012;109(6). CrossRef
- Partial cystectomy for muscle invasive urothelial carcinoma of the bladder: a contemporary review of the M. D. Anderson Cancer Center experience Kassouf W, Swanson D, Kamat AM , Leibovici D, Siefker-Radtke A, Munsell MF , Grossman HB , Dinney CPN . The Journal of Urology.2006;175(6). CrossRef
- Partial cystectomy: a contemporary review of the Memorial Sloan-Kettering Cancer Center experience and recommendations for patient selection Holzbeierlein JM , Lopez-Corona E, Bochner BH , Herr HW , Donat SM , Russo P, Dalbagni G, Sogani PC . The Journal of Urology.2004;172(3). CrossRef
- Role of partial cystectomy for muscle invasive bladder cancer: Impact on morbidity and overall survival, a population-based study, 2006-2017 Posielski N, Koenig H, Jung N, Ho O, Flores JP , Porter C. 2021;39(15_suppl):e16530-e16530. CrossRef
- Partial cystectomy does not undermine cancer control in appropriately selected patients with urothelial carcinoma of the bladder: a population-based matched analysist Capitanio U, Isbarn H, Shariat SF , Jeldres C, Zini L, Saad F, et al . Urology.2009;74(4). CrossRef
- The impact of routine frozen section analysis during partial cystectomy for bladder cancer on surgical margin status and long-term oncologic outcome. Urol Oncol Semin Orig Investig [Internet] Sharma M, Nagata Y, Yang Z, Miyamoto H. 2020.2020;38(12):e1-933.e6. CrossRef
- Laparoscopic partial cystectomy for urachal and bladder cancer Colombo JR , Desai M, Canes D, Frota R, Haber G, Moinzadeh A, Tuerk I, et al . Clinics (Sao Paulo, Brazil).2008;63(6). CrossRef
- Is frozen section analysis of the urethra at the time of radical cystectomy and orthotopic neobladder urinary diversion mandatory? Sureka SK , Yadav A, Arora S, Kapoor R, Mandhani A. Indian Journal of Urology : IJU : Journal of the Urological Society of India.2015;31(4). CrossRef
- Robot-assisted partial cystectomy with intraoperative frozen section examination: Evolution and evaluation of a novel technique Sood A, Klett DE , Abdollah F, Sammon JD , Pucheril D, Menon M, Jeong W, et al . Investigative and Clinical Urology.2016;57(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times