Painless Endoscopic Repair of Duodenal Ulcer Perforation: A Case Report
Download
Abstract
This paper reports a case of duodenal ulcer (A1 stage) after general gastroscopy, when the patient left hospital without discomfort, but felt persistent aggravated abdominal pain in about 20 minutes, so admitted to the emergency department due to perforation of duodenal ulcer showed by CT, and aspirated by CO2 air pump under general anesthesia in the operating room four hours later, performed painless endoscopic perforation repair. Then, he released pneumatosis by puncture, and accepted ten days symptomatic treatment such as anti-infection following fasting water and gastric tube insertion, after that recovered and discharged from hospital, avoiding surgery, which supplements endoscopic minimally invasive treatment for perforation of duodenal ulcer in China.
Introduction
The patient, male, 68 years old, was admitted to hospital at 12:00 am on October 19, 2022 because of “black stool for 9 days and abdominal pain for 1 hour”. Nine days ago, the patient had black mushy stool without obvious inducement, 2-4 times/day, no hematemesis, no abdominal pain and distension, occasional dizziness, palpitation, aggravation after activities, no chest tightness and asthma. His stool gradually turned yellow after went to a local hospital for symptomatic treatment. At 10:40, he went to our hospital today for further diagnosis and treatment, the general gastroscopy showed that the duodenal bulb was deformed with diverticulum-like changes. An ulcer with a diameter of about 1.5 cm could be seen in the anterior wall of the bulb, with deep bottom and black blood scab in the center, surrounded by yellow and white moss and mucous membrane congestion and edema. No abnormality was found in the descending part. At about 11:00, the patient suddenly suffered from tear-like pain in the upper abdomen, then admitted to the digestive department as “abdominal pain” in emergency department with the worsen condition and the curled-up position was slightly relieved.
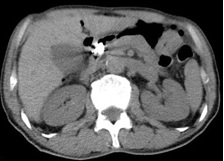
He had no previous history of cardiovascular and cerebrovascular diseases, infectious diseases, drug and food allergy. Also no special in personal, marriage and childbearing and family history. Specialized physical examination indicated: clear mind, poor spirit, shortness of breath, chest breathing; abdominal bulge, plate abdomen, refusal to press, total abdominal tenderness and rebound pain. After admission, emergency CT showed perforation of duodenal ulcer. As shown in Figure 1.
Figure 1. Free Gas in Abdominal Cavity Can be Seen.

After admission, it was found emergency WBC 4.44*109/L, HGB 104G/L, GRAN% 78.9%, CRP 64MG/L, residual blood coagulation, liver function and electrolyte were normal following emergency treatment was given,such as fasting water, acid inhibition and stomach protection. In terms of emergency gastrointestinal surgery consultation, emergency surgery was recommended, but endoscopic examination under general anesthesia in operating room was determined, considering that potentially perforated after ordinary gastroscope may lead to disputes, and endoscopic treatment is given if necessary.
At 15:30 pm, the endotracheal intubation and CO2 air pump were used in the operating room under general anesthesia. When entering the duodenum, bulbar deformation and diverticulum-like changes were seen.
Ulcer perforation was observed in the anterior wall of the large curved side, with a diameter of about 6MM. Five harmonious clips with an opening of 1.4 CM and a purse suture with a nylon rope perforation were performed. As shown in Figure 2A-B, the operation lasted about 45 minutes. After the operation, the patient was punctured by a syringe and deflated in the abdominal cavity due to abdominal bulge as seen in Figure 2B, and placed a gastric tube.
Figure 2. a. Perforation Size is about 6MM, b. Abdominal Puncture Deflation.

The first day after operation
The symptoms of abdominal pain were slightly improved, abdominal distension, anal exhaust and defecation stopped, but fever occurred, with the highest body temperature of 38.6 ℃. The related indexes showed that WBC 7.81*109/L, HGB 97G/L, GRAN% 84.2%, CRP 206MG/L, PCT 1.77 NG/ML continued to be treated with acid inhibition, stomach protection, inhibition of intestinal secretion and anti-infection.
The second day after operation
The patient felt better than before, with slight abdominal distension, no exhaust and defecation in anus, the highest body temperature of 38.7 oC, recovered after antipyretic symptomatic treatment. The relevant indexes showed that WBC 11.42*109/L, HGB 101G/L, GRAN% 86.20%, CRP 264MG/L, with better symptoms were than before, but the infection was not controlled.
Day 4 after operation
The patient had no abdominal pain, felt abdominal distension relief during quiet rest, and the anus had spontaneous exhaust and defecation. The related indexes showed that white blood cells were normal, WBC 5.21*109/L, GRAN% 51.4%, CRP 80MG/L, and the indexes and symptoms were better, so CT could be reexamined at an optional time.
Day 5 after operation
CT suggested that postoperative changes of duodenal bulb were visible, with a small amount of free gas found in Figure 3.
Figure 3. After Treatment, the Abdominal Gas Decreased and Titanium Clips was Clamped in Place.
Patients try drinking water, and eat liquid food if no abnormality. On the 10th day after operation, the patient had no obvious abnormality, with normal intestinal function, then discharged from hospital.
Discussion
Peptic ulcer is a common disease of upper digestive tract, including gastric ulcer (GU) and duodenal ulcer (GU), which leads to bleeding and perforation, the common complications. However, duodenal ulcer perforation is rare in clinic, accounting for 2%-20% of the total ulcer perforation, which often threatens patients’ lives. Related studies show that its mortality rate can reach 10%-40% [1-3]. Risk factors for perforation include H. PYLORI infection, long-term use of non-steroidal anti-inflammatory drugs, and iatrogenic perforation such as endoscopic retrograde cholangiopancreatography [4-7]. As the most common occurred in the anterior wall of duodenal bulb, the perforation of duodenal ulcer may be caused by the anterior wall goes straight to the peritoneal cavity, and not easy to adhere due to respiration and diaphragm movement; Secondly, the anterior wall is relatively empty without other organs that not easy to adhere if perforated; Thirdly, the wall of the tube is thin, and the blood supply relatively fewer, mainly comes from the branches of pancreatic and gastroduodenal arteries [8]. Treatment includes conservative, endoscopic minimally invasive and surgical treatment. The conservative treatment should be strictly selected according to the patient’s age, whether it is complicated with basic diseases, perforation site, time, abdominal symptoms and signs, and must meet the following conditions: (1) perforation caused by non-malignant ulcer; (2) The age is less than 70 years old; (3) The overall condition was stable without serious complications (ASA-PS grade 1 or grade 2).
(4) Imaging showed that ascites was confined to the upper abdomen. (5) No obvious signs and symptoms of peritonitis; (6) The perforation diameter is less than 5MM [9]. A Swiss study reported that 12 out of 398 patients received conservative treatment; Eight of them died of various complications [10]. Surgical operations, including laparoscopy and laparotomy, are also the classic and common surgical methods for perforation of duodenal ulcer, with generally good prognosis. It is now not reported a successful case of endoscopic repair of duodenal ulcer perforation in China, but self-expanding metal stents was used to perform endoscopic stent implantation for perforated patients by some foreign scholars, including 3 cases had abdominal leakage after surgery and underwent stent implantation, and the rest of the patients used stent implantation and abdominal drainage because they couldn’t tolerate surgery. Although they recovered after surgery, they had great trauma, long hospitalization time, easy stent falling off, sealing duodenal papilla opening, etc., and had poor effect on the anterior wall of duodenal bulb, so the operation has limited clinical application [11]. This patient in the study had black stool and abdominal pain after long-term oral administration of non-steroidal anti-inflammatory drugs, and his stool turned yellow after 10 days of treatment in the local hospital, then was found a deep and large ulcer in the anterior wall of duodenal bulb after came to our hospital for general gastroscopy. The abdominal pain became worse about 20 minutes after withdrawal of the endoscope, then perforation was considered due to the abdomen was plate, which was confirmed by CT. Possible causes of perforation include: (1) deep ulcer; (2) The severe stimulation during gastroscopy leads to severe contraction and relaxation of gastrointestinal tract and stimulates ulcer perforation; (3) Because of deformed duodenal bulb and obvious edema, as well as violently touching the ulcer surface when entering the endoscope. There is no sign of conservative treatment because old age and large ulcer perforation area located on the front wall, as well as obvious peritonitis and obvious free gas in abdominal cavity showed by CT. However, the choice of surgery may involve disputes, therefore, painless endoscopic repair of duodenal ulcer perforation was performed under general anesthesia in operating room with C02 air pump, making the patient cured and discharged from hospital. At present, there is no successful case of endoscopic treatment of duodenal ulcer perforation in China, of which the difficulty and skill contains: the ulcer area is large and deep, surrounded by congestion, edema and deformation located in the anterior wall of the ball (1) near the pylorus, the operable space under endoscope is so limited that the titanium clip is hardly accommodated; (2) The ulcer surface is stiff, surrounded by edema, which is too brittle to effectively clamp the mucosa by the titanium clip, so leading to bleed repeatedly when touching the mucosa; (3) there is no support point when endoscope enters into the narrow duodenal bulb space is, resulting in the endoscope can not be fixed on the perforation surface. Necrotic tissues and few fresh blood vessels in perforation may lead to failure to heal, further cause serious adverse consequences due to missing the best operation opportunity. Tip: Fix nylon rope to the normal mucosa around the ulcer with a titanium clip. Then, the other four titanium clips uniformly clamp the oval nylon rope to fix around the ulcer, slowly shrink the nylon rope to suture the perforated purse. At this time, do not violently entering but observe the purse suture where is no space in the ball, as well as dynamically observation on the symptoms and inflammatory indicators of the patient after pulling out the gastroscope.
References
- Management of duodenal perforation post-endoscopic retrograde cholangiopancreatography. When and whom to operate and what factors determine the outcome? A review article Machado NO . JOP: Journal of the pancreas.2012;13(1).
- Multicentre trial of a perioperative protocol to reduce mortality in patients with peptic ulcer perforation Møller MH , Adamsen S., Thomsen RW , Møller AM . The British Journal of Surgery.2011;98(6). CrossRef
- Systematic review of the epidemiology of complicated peptic ulcer disease: incidence, recurrence, risk factors and mortality Lau Jy , Sung J, Hill C, Henderson C, Howden CW , Metz DC . Digestion.2011;84(2). CrossRef
- Strategies to improve the outcome of emergency surgery for perforated peptic ulcer Søreide K, Thorsen K, Søreide JA . The British journal of surgery.2014;101(1). CrossRef
- A systematic review of the management and outcome of ERCP related duodenal perforations using a standardized classification system Cirocchi R, Kelly MD , Griffiths EA , Tabola R, Sartelli M, Carlini L, Ghersi S, Di Saverio S . The Surgeon: Journal of the Royal Colleges of Surgeons of Edinburgh and Ireland.2017;15(6). CrossRef
- Perforated peptic ulcer - an update Chung KT , Shelat VG . World Journal of Gastrointestinal Surgery.2017;9(1). CrossRef
- Peptic ulcer disease Lanas A, Chan Fkl . Lancet (London, England).2017;390(10094). CrossRef
- Risk factors of duodenal ulcer with perforation Chao Y, Wu D. Journal of North Sichuan Medical College.2021;36(11):1479-1483.
- A pilot study to evaluate the effectiveness and safety of urgent endoscopy for gastroduodenal perforation Asayama N, Nagata S, Kano M, Shigita K, Aoyama T, Fukumoto A, Mukai S. Surgical Endoscopy.2022;36(4). CrossRef
- [Conservative treatment of gastroduodenal peptic ulcer perforations: indications and results] Alizadeh N., Bühler L., Huber O., Morel P.. Schweizerische Medizinische Wochenschrift. Supplementum.1997;89.
- Self-expandable metal stents as a new treatment option for perforated duodenal ulcer Bergström M., Arroyo Vázquez JA , Park PO . Endoscopy.2013;45(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times