Low Dose Daily Cisplatin vs Weekly Dose Cisplatin in Radiation Therapy for Head and Neck Squamous Cell Carcinoma, A Comparative Study
Download
Abstract
Introduction: Head and neck cancer is prevalent in India’s North and North Eastern regions, often treated with concurrent cisplatin-based chemo-radiation therapy. This study compares the efficacy, side effects, and toxicities of daily low-dose cisplatin versus weekly high-dose cisplatin in head and neck cancer patients receiving radiation therapy. Objective: To assess the efficacy and compare the toxicities of daily versus weekly cisplatin dosing in concurrent chemo-radiation therapy.
Materials and Methods: A study of 139 patients with biopsy-proven head and neck squamous cell carcinoma was conducted at Assam Medical College from October 2022 to August 2024. Patients were assigned to either daily (ARM A) or weekly (ARM B) cisplatin regimens. Toxicities were graded using RTOG criteria, and tumour response was assessed with RECIST criteria.
Results: ARM A showed a higher complete response (56%) compared to ARM B (49%). ARM A had lower acute toxicities, including dysphagia and mucositis( p value < 0.05). Both regimens showed similar weight loss and low rates of nephrotoxicity.
Conclusion: Daily low-dose cisplatin offers similar efficacy with fewer severe acute toxicities, making it a preferable option for head and neck cancer patients.
Introduction
Head and neck cancer is a significant global health burden. In India Head and neck cancer occurs especially in the North and North Eastern parts due to the consumption of tobacco and related products and the life style modifications associated. Radiation therapy has become one of the standards of treating Head and Neck cancers, be it definitive, concurrent or as adjuvant after surgery [1]. As of now cisplatin has become the gold standard chemotherapeutic agent with the preferred three-weekly dose along with Radiation therapy as definitive even-though multiple studies have shown the efficacy of Low dose over High dose cisplatin [2, 3]. A study by Marcus et al, showed administering cisplatin daily improves tumour control by 35% compared to radiation alone, while weekly dosing yields only a 6% improvement [4]. In this study, we compared the head and neck cancer patients receiving radiation therapy with concurrent daily dose cisplatin vs weekly dose cisplatin.
Aim
Observational comparative assessment of treatment prognosis ,side-effects and toxicities with low dose weekly cisplatin and daily dose cisplatin for head and neck cancer patients receiving radiation therapy
Objectives
1) To access the efficacy of cisplatin as a daily dose and with weekly doses.
2) To compare the toxicities and side effects with cisplatin as a daily dose and weekly dose.
Materials and Methods
Single institutional study at Assam Medical College in-order to rule out discrepancies with institutional protocols and treatment set-ups.This prospective cohort study was designed in accordance with the STROBE guidelines to ensure comprehensive reporting of study methods, results, and limitations. The study was done from October 2022 to August 2024.
Inclusion Criteria
a) Biopsy proven squamous cell carcinoma patients limited to oral cavity, oropharynx, hypopharnyx, nasopharnyx, larynx who will receive radiation therapy as either adjuvant, definitive or concurrently with Cisplatin.
b) Age 18-70 , with no major co-morbidity.
c) Karnofsky scale => 70
d) Informed written Consent. Exclusion Criteria :
a) Patients already treated with radiation therapy in the past.
b) Cancers other than squamous cell carcinoma
c) Cancer of nasal cavity or sinuses or unknown primary
d) Patients that received induction chemotherapy or neo-adjuvant chemotherapy before starting on radiation therapy.
e) Karnofsky scale <70.
f) Poor General Conditions.
Methodology
All Patients fulfilling the inclusion and exclusion criteria, who undertook radiation therapy with cisplatin for head and neck squamous cell carcinoma during the study period, where divided into 2 arms upon observation.
ARM A = Daily dose cisplatin ARM B = weekly dose cisplatin
Plan of Study
ARM A Chemotherapy Schedule:
CDDP/ Cisplatin Injection of 6mg/m2 (maximum up to 10mg) diluted in 100ml 0.9 % NS, given over 20 minutes , 30 minutes before RT everyday (Monday to Friday) after weekly CBC and RFT investigations are within normal limits. Taken as OPD basis.
ARM B Chemotherapy Schedule:
CDDP/ Cisplatin Injection of 40mg/m2 (maximum up to 50mg) diluted in 500ml 0.9 % NS, given over 2hrs, weekly once ( preferably on Monday or Tuesday) before radiation therapy after weekly CBC and RFT investigations are within normal limits. Taken as in-patient after hydration with 500ml NS, followed by infusion Mannitol 20% , 1g of Magnesium sulphate and 20meq of KCl ( Potassium chloride) infusion wherever necessary. The patients in both the arms received radiation doses ranging from 60-70 Gy in 30-35 fractions as conventional radiation therapy using Bhabhatron -II Telecobalt machine with appropriate immobilisation devices and cord reductions. None of the patients were under scrutiny for gap corrections.
Toxicity and side effect evaluation will be based on RTOG [5] grading, while tumour response was based on RECIST criteria [6, 7] with appropriate radiological investigations done at follow up period.
Statistical analysis
Statistical analysis was done using SPS v25.0, and CHI square test was done to determined associations. P value of less that 0.05 was determined to be statistically significant.
Results
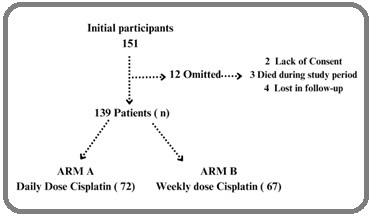
Total of 151 patients were initially enrolled in the study, with 139 completing the treatment. Twelve patients were lost to follow-up, died during treatment, or opted out. The cohort was divided into ARM A (daily Cisplatin, 72 patients) and ARM B (weekly Cisplatin, 67 patients). The mean age of patients in ARM A was 47 years, while in ARM B it was 49 years. Both arms were predominantly male (58.3% in ARM A and 64.2% in ARM B). The most common primary cancer sites were the oral cavity and oropharynx. Radiation doses were predominantly 70 Gy, with ARM A receiving an average dose of 68.3 Gy and ARM B receiving 67.7 Gy. Acute toxicity profiles showed that 55% of ARM A patients experienced Grade III/IV dysphagia, in contrast to 91% in ARM B. Additionally, 46% of ARM A patients developed Grade III/IV mucositis, compared to 81% in ARM B. Anaemia and leukopenia were more prevalent in ARM B, with 12% of patients in this group experiencing Grade II anaemia and 27% having Grade I/II leukopenia. Both arms reported similar median weight loss of 4 kg. Regarding late toxicities observed 4-6 months post-treatment, dysphagia (Grade II/III) occurred in 18% of ARM A patients and 27% of ARM B patients. Xerostomia (Grade II/III) was more common in ARM B (45%) than in ARM A (32%). Nephrotoxicity and ototoxicity were minimal in both arms. In terms of clinical outcomes, ARM A exhibited a higher complete response rate (56%) compared to ARM B (49%), while partial response rates were consistent across both arms (24%). Stable disease was observed in 13% of ARM A patients and 15% of ARM B patients, while 8% in ARM A and 12% in ARM B experienced progressive disease (Figure 1) (Table 1-5).
Figure 1. Initial Patient and Consort Diagram.
| Characteristic | ARM A | ARM B | Total |
| daily dose (72- patients) | weekly dose (67 patients) | (n = 139) | |
| Age (mean) | 47 | 49 | |
| Median, years | 45 | 48 | |
| Sex No (%) | |||
| Male | 42 (58.3%) | 43 (64.2%) | |
| Female | 30 (41.6) | 24 (35.8%) | |
| Primary site No (%) | |||
| Oral cavity | 20 (27.7) | 18 (26.8) | |
| Oropharynx | 18 (25) | 20 (29.8) | |
| Larynx | 13 (18) | 11 (16.4) | |
| Hypopharynx | 16 (22.2) | 15 (22.3) | |
| Nasopharnyx | 5 (6.9) | 3 (4.4) | |
| T stage No (%) c | |||
| T1 | 4 (5) | 3 (4.4) | |
| T2 | 12 (16.6) | 12 (17.9) | |
| T3 | 30 (41.6) | 26 (38.8) | |
| T4 | 26 (36.1) | 22 (32.8) | |
| N stage No (%) | |||
| N0 | 15 (20.8) | 17 (25.3) | |
| N1 | 21 (29.1) | 18 (22.3) | |
| N2 | 30 (41.6) | 28 (41.7) | |
| N3 | 6 (8) | 4 (5.9) | |
| TNM stage | |||
| Planned CRT modalities | |||
| Definitive | 51 (70.9) | 42 (62.6) | 93 (67) |
| Post-operative | 21 (29.1) | 25 (37.3) | 46 (33) |
| RT dose (Conventional) | ARM A | ARM B |
| 70 Gy - n (%) | 51 (70.9) | 42 (62.6) |
| 66 Gy- n (%) | 15 (20.8) | 16 (23.8) |
| 60 Gy- n (%) | 6 (8.3) | 9 (13.4) |
| Mean Dose | 68.3 Gy | 67.7 Gy |
| Acute Toxicities Observed by nearing end of treatment | Grade (WHO) | Arm A (n) (%) | Arm B (n) (%) | P value |
| Dysphagia | Grade II | 20 (28) | 3 (4) | |
| Grade III/IV | 40 (55) | 61 (91) | 6.78 × 10⁻⁶ | |
| Mucositis | Grade I/II | 5 (7) | 15 (22) | |
| Grade III/IV | 33 (46) | 54 (81) | 4.97 × 10⁻⁵ | |
| Anaemia | Grade I | 9 (13) | 15 (22) | |
| Grade II | 2 (3) | 8 (12) | 0.078 | |
| Leukopenia | Grade I/II | 12 (17) | 18 (27) | |
| Grade III | 6 (8) | 6 (9) | 0.21 | |
| Weight loss (kg, median) | 4 (6) | 4 (6) | - |
| Late Toxicities observed at 4–6 months from initial treatment | Arm A (n, %) | Arm B (n, %) | p value |
| Dysphagia (Grade II/III) | 13 (18) | 18 (27) | 6.78 × 10⁻⁵ |
| Xerostomia (Grade II/III) | 23 (32) | 30 (45) | 0.167 |
| Nephrotoxicity | 2 (3) | 2 (3) | 1 |
| Ototoxicity | 3 (4) | 4 (6) | 0.922 |
| Follow- up at 6months-8 months after initial treatment | Arm A (n = 72, daily low-dose chemotherapy) | Arm B (n = 67, weekly-dose chemotherapy) | P value |
| Complete Response (CR) | 40 (56%) | 33 (49) | 0.566 |
| Partial Response (PR) | 17 (24%) | 16 (24%) | 1 |
| Stable Disease (SD) | 9 (13%) | 10 (15%) | 0.866 |
| Progressive Disease (PD) | 6 (8%) | 8 (12%) | 0.566 |
ARM A (Daily dose cisplatin Group) had 72 patients. (51.8 %) ARM B (Weekly cisplatin Group) had 67 patients. (48.2 %)
Discussion
This study was designed to evaluate the efficacy and toxicity profiles of daily low-dose cisplatin compared to weekly high-dose cisplatin in head and neck cancer patients undergoing radiation therapy. Our findings suggest that while both regimens achieve similar efficacy in terms of tumour response, they exhibit distinct differences in side effects and overall toxicity.
The role of cisplatin as a Radio-sensitizer is crucial for enhancing the effectiveness of radiation therapy. In our study, Arm A (daily Cisplatin) achieved a 56% complete response (CR), which is 7% higher than Arm B, which had a 49% CR rate. However, the difference in CR rates between the two groups was not statistically significant (p = 0.566). Both treatment arms showed similar partial response (PR) rates of 24%, stable disease (SD) at 13% (Arm A) vs. 15% (Arm B), and progressive disease (PD) at 8% (Arm A) vs. 12% (Arm B), all of which were not statistically significant (p > 0.05). This aligns with findings from Prabhash et al. (2014), which reported no significant difference in CR rates between different cisplatin regimens in head and neck cancer patients [8].
Toxicity and Side Effects
Toxicity remains a significant concern in Cisplatin- based regimens. Arm A (daily Cisplatin) reported substantially lower rates of acute mucositis and dysphagia compared to Arm B (weekly Cisplatin). Specifically, 55% of Arm A patients developed Grade III/IV dysphagia, while 91% of patients in Arm B experienced severe dysphagia, a statistically significant difference (p = 6.78 × 10⁻⁶). Similarly, 46% of Arm A patients had Grade III/IV mucositis, compared to 81% in Arm B (p = 4.97 × 10⁻⁵). These findings are consistent with Tsan & Pang (2010), which also reported significantly higher rates of acute mucositis and dysphagia in weekly cisplatin regimens [3]. Other toxicities, such as leukopenia (p = 0.210), anaemia (p = 0.078), and Xerostomia (p = 0.167), were not statistically significant between the two groups. This supports findings from Marcus et al. (2004), who found that haematological toxicities did not differ significantly between different cisplatin dosing schedules [4].
Renal and Ototoxicity
Both regimens showed low rates of nephrotoxicity (3% in both arms) and ototoxicity (4% in Arm A vs. 6% in Arm B). The differences in nephrotoxicity (p = 1.000) and ototoxicity (p = 0.922) were not statistically significant. These results align with findings from Vermorken & Trigo (2012), which reported minimal nephrotoxicity differences between daily and weekly cisplatin regimens [1].
Despite extensive research comparing high-dose cisplatin to either weekly or daily low-dose regimens, there remains limited literature directly comparing two low-dose schedules weekly and daily Cisplatin for HNSCC. Most studies have focused on the differences between high-dose and low-dose regimens rather than evaluating whether daily low-dose cisplatin provides a distinct advantage over weekly low-dose regimens in terms of toxicity and efficacy. Our study addresses this gap by directly comparing these two low-dose strategies, highlighting that daily cisplatin significantly reduces severe acute toxicities such as dysphagia and mucositis, without compromising treatment efficacy. Previous studies have examined weekly and high-dose regimens, with Ameri et al. (2020) finding that weekly cisplatin regimens lead to fewer acute toxicities than three-weekly schedules, though they still carry a significant risk of mucositis and dysphagia [9]. Similarly, Fan et al. (2018) compared acute toxicities in different Cisplatin-based chemo-radiation regimens and concluded that weekly regimens might offer a more favourable toxicity profile compared to the three-weekly approach, although daily low-dose regimens remain under-explored [10]. Furthermore, Le (2021) discussed the optimal cisplatin regimen for head and neck cancer, suggesting that while weekly dosing may be effective, the precise regimen that minimizes toxicity while maintaining efficacy is still to be determined [11]. Further randomized controlled trials are needed to confirm these findings and establish an optimized low-dose cisplatin schedule for head and neck cancer patients.
Limitations of the study
1. Selection bias, as it is a single institutional study.
2. Strict exclusion criteria hence not reflecting real world scenarios ( where most patients have been treated with prior chemotherapy).
3. Limited study period to access long term side-effects like fibrosis or in-field recurrences or relapses.
In conculsion, this study demonstrates that while both daily and weekly cisplatin regimens offer similar efficacy, weekly cisplatin is associated with significantly higher rates of severe dysphagia and mucositis (p < 0.0001). Non-significant findings for anaemia, leukopenia, nephrotoxicity, and ototoxicity suggest that both regimens remain viable options depending on patient tolerance. Given its lower acute toxicity, daily cisplatin may be the preferred regimen for better patient adherence and outpatient management.
Aknowledgments
1. This research did not receive any specific grant from funding agencies in the public, commercial, or not- for-profit sectors.
2. The authors declare no conflict of interest.
References
- Cisplatin-based chemotherapy in the management of head and neck cancer Vermorken JB , Trigo JM . Journal of Clinical Oncology.2012;30(4):398-404.
- Efficacy of chemotherapy and radiation in combination for head and neck cancer List MA , Boles R. Cancer Treatment Reviews.;28(6):379-390.
- Toxicity profiles of weekly versus three-weekly cisplatin in concurrent chemoradiation for head and neck cancer: A systematic review Tsan CT , Pang WW . European Journal of Cancer.2010;46(10):1724-1732.
- Concurrent chemoradiotherapy in the treatment of locally advanced head and neck cancer Marcus SL , et al . Cancer Journal.2004;10(3):177-186.
- RTOG (Radiation Therapy Oncology Group). Radiation therapy oncology group: Acute and late radiation morbidity scoring criteria. American College of Radiology 1995.
- New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eisenhauer E. A., Therasse P., Bogaerts J., Schwartz L. H., Sargent D., Ford R., Dancey J., et al . European Journal of Cancer (Oxford, England: 1990).2009;45(2). CrossRef
- Low-dose daily cisplatin combined with radiation therapy in the treatment of advanced head and neck squamous cell carcinoma: A randomized trial Jeremic B, Shibamoto Y. International Journal of Radiation Oncology, Biology, Physics.1998;40(2):367-374.
- Toxicity and treatment outcomes of concurrent chemoradiotherapy for locally advanced squamous cell carcinoma of the head and neck: A revie Prabhash K, Bhosale S. Indian Journal of Cancer.2014;51(3):234-240.
- Randomized trial on acute toxicities of weekly vs. three-weekly Cisplatin-based chemoradiation in head and neck cancer Ameri A, et al . Journal of Clinical Oncology.2020;38(3):234-242. CrossRef
- Comparison of acute toxicities in two primary chemoradiation regimens in the treatment of advanced head and neck squamous cell carcinoma Fan KY , et al. . Head & Neck.2018;40(7):1563-1570. CrossRef
- Optimal regimen of cisplatin in squamous cell carcinoma of the head and neck yet to be determined Le X. Cancer Chemotherapy and Pharmacology.2021;87(4):511-518. CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times