A Case of Chronic Myeloid Leukemia Presenting with Osteoid Osteoma: A Diagnostic Dilemma
Download
Abstract
Chronic myeloid leukemia is a hematological malignancy resulting from a clonal proliferation of hematopoietic stem cells of the myeloid series. It is developed by chromosomal translocation. Chronic Myeloid Leukemia (CML) usually occurs in adults and is rare in children. Osteoid osteoma is a benign bone lesion with no malignant potential. The association of chronic myeloid leukemia with osteoid osteoma is not reported in the literature. An atypical presentation of osteoid osteoma may complicate the diagnosis when associated with a primary malignancy. In this report, we have discussed a case of atypical presentation of osteoid osteoma suspected to be a lytic bone lesion in CML.
Introduction
Chronic myeloid leukemia (CML) is a clonal hematopoietic disorder, accounting for 15% of all leukemia. According to the SEER program, the median age of diagnosis is 66 years, which is much higher than reported in many trials [1]. The disease is usually seen in adults in the age group of 50 to 60 years, with a slight male predominance [2]. The discovery of the Philadelphia chromosome in 1960 made CML the first neoplasm to be characterized by cytogenetic marker [3]. The only risk factor for the development of CML is exposure to high radiation doses and is evident from survivors of the atom bomb explosion in Japan in 1945 and follow-up of patients treated with radiation for ankylosing spondylitis and cervical cancer [4].
Osteoid osteoma is a benign bone tumor diagnosed usually in males in the age group of 5-35 years [5]. It is usually found in the long bones of extremities and presents with long-standing history of pain, typically nocturnal pain, which is relieved by salicylates [6]. Rare location and atypical radiological presentation may delay the diagnosis and treatment [7]. Here we report a case of CML that presented with osteoid osteoma at a rare site.
Case Description
A 54-year-old female patient, a known case of CML with a clinical history of leukocytosis, hepato-splenomegaly, and BCR-ABL positive for the last 8 months was referred to us for evaluation of a two weeks history of back and right gluteal region pain which was aggravated by movement and relieved on lying prone. On examination, there was extreme tenderness over the right side of the sacrum, the straight leg raising test was positive, and hip movement was painful. CT (Computed Tomography) scan suggested a lytic lesion in the right ala of the sacrum. We suspected this to be a bone involvement in CML and started the patient on pain medicines and the first dose of zoledronic acid and sent for further investigation.
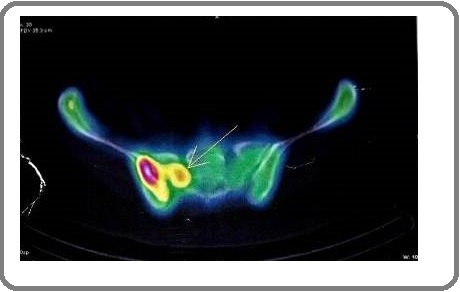
PET CT suggested increased metabolic activity in the right sacral ala (Figure 1).
Figure 1. PET- CT Showing Increased Metabolic Activity in Right Sacral Ala.
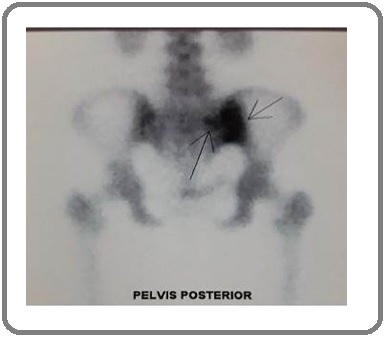
Bone scintigraphy reported a fairly well-defined radiolucent area surrounded by sclerotic rim showing increased uptake in right sacral ala at S2 vertebral level, and the lesion was suspected to be an osteoid osteoma (Figure 2).
Figure 2. Bone Scintigraphy Image of the Sacral Ala Lesion (marked by black arrows).
A needle biopsy was done which reported features of woven bone and the presence of osteoblasts and osteoclasts, thus, supporting the findings of bone scintigraphy. After a confirmatory diagnosis of the benign condition, the patient was referred to the department of orthopedics for further treatment.
Discussion
Chronic myeloid leukemia is a biphasic or triphasic illness. The disease can progress to more aggressive leukemia as a malignant clone loses the capacity for terminal differentiation. BCR-ABL TKI is the standard frontline therapy for newly diagnosed cases of the chronic phase of chronic myeloid leukemia [8]. Allogenic HCT is reserved for patients with resistance to TKI or management of advanced phase due to its morbidity and mortality. Cases of secondary malignancy are very few in the literature. Secondary primary malignancy of the breast, neuroendocrine tumor of the caecum, squamous cell carcinoma of the skin, acute lymphocytic leukemia have been reported but there has been no case of any benign tumor being reported in the literature [9-11]. Elmhadi et al reported a case of successful management of synchronous recurrent breast carcinoma with chronic myelogenous leukemia [12]. Pan L et al reported a case of secondary breast carcinoma after completely remitted chronic myeloid leukemia following targeted tyrosine kinase therapy [13]. Campione E et al reported a case of Kaposi sarcoma in a patient treated with imatinib mesylate for chronic myeloid leukemia [14].
Treatment of osteoid osteoma comprised of conservative management to excision and newer techniques like radiofrequency ablation [6]. Osteoid osteoma is a benign condition and its malignant transformation has not been reported in the literature [15]. However, various atypical presentations of the benign tumor may delay diagnosis, especially when associated with a malignant condition [7]. The typical presentation of osteoid osteoma is a long-standing history of pain which is relieved by salicylates, male sex, and an age group of 5-35 years. 50% are located in the long bones of the extremity with the least common locations being skull, pelvis, ribs scapula, etc. [7]. Typical CT scan finding is a central nidus with variable attenuation and surrounding sclerosis [16]. Various atypical features like bone destruction, marrow edema, periosteal reaction, sclerosis obscuring nidus, and complete sclerotic lesion may obscure the diagnosis [7]. Our patient had presented at an age of 54 years, with a short 2 weeks history. CT findings show a right sacral ala lytic lesion. Older age of presentation, sacral location, and lytic lesion on CT are not typical findings of osteoid osteoma-which led to diagnostic delay. Moreover, its association with CML complicated the picture. Various case reports and series in the literature have reported a solitary lytic bone lesion in CML (17–20). These lesions usually precede a blastic phase and suggest a poor prognosis. A lytic lesion in CML is usually treated with hypofractionated radiotherapy for pain and pain medications according to the WHO pain ladder. Thus, an atypical presentation of osteoid osteoma and an association with CML complicated the diagnosis of osteoid osteoma. There is one case report in the literature that reported an intracortical bone metastasis presenting with features of intracortical osteoid osteoma in a patient with lung adenocarcinoma [21]. Thus, a bone lesion in a patient with a primary malignancy should call for an extensive investigation to rule out metastatic or malignant disease. A CML co-presenting with osteoid osteoma has not been reported in the literature. Our case is unique because the presentation was at a rare site with atypical CT features complicating the diagnosis. We may also conclude that a tissue diagnosis should always be carried out in a bone lesion with an associated primary malignancy.
In conclusion, chronic myeloid leukemia is a hematological malignancy and its presentation with osteoid osteoma has not been seen in the literature. An atypical presentation of the benign bone lesion may complicate the diagnosis and should be confirmed by histopathology.
Ethics Approval, Statement of Compliance, and Clinical Trial Transparency
Ethical committee approval was taken for the publication of this document. Informed consent of the patient was taken for the publication of clinical findings.
Abbreviations
CML- Chronic Myeloid Leukemia, CT- Computed Tomography
References
- Epidemiology of chronic myeloid leukaemia (CML) Rohrbacher Maren, Hasford Joerg. Best Practice & Research Clinical Haematology.2009;22(3). CrossRef
- Summary of the published Indian data on chronic myeloid leukemia Singhal Manish K., Sengar Manju, Nair Reena. South Asian Journal of Cancer.2016;05(03). CrossRef
- The minute chromosome (Ph1) in chronic granulocytic leukemia Nowell C.. Blut Zeitschrift für die Gesamte Blutforschung.1962;8(2). CrossRef
- Mortality from cancer and other causes after radiotherapy for ankylosing spondylitis. Brown W. M., Doll R.. BMJ.1965;2(5474). CrossRef
- Osteoid Osteoma Boscainos Petros J., Cousins Gerard R., Kulshreshtha Rajiv, Oliver T. Barry, Papagelopoulos Panayiotis J.. Orthopedics.2013;36(10). CrossRef
- Osteoid osteoma: Contemporary management Noordin Shahryar, Allana Salim, Hilal Kiran, Nadeem Naila, Lakdawala Riaz, Sadruddin Anum, Uddin Nasir. Orthopedic Reviews.2018;10(3). CrossRef
- Osteoid osteoma: the great mimicker Carneiro Bruno C., Da Cruz Isabela A. N., Ormond Filho Alípio G., Silva Igor P., Guimarães Júlio B., Silva Flávio D., Nico Marcelo A. C., Stump Xavier M. G. R. G.. Insights into Imaging.2021;12(1). CrossRef
- How I treat chronic myeloid leukemia in the imatinib era Goldman John M.. Blood.2007;110(8). CrossRef
- Second primary malignancies in chronic myeloid leukemia patients Eskazan AhmetEmre, Caliskan Tugce. Journal of Cancer Research and Therapeutics.2015;11(4). CrossRef
- Neuroendocrine tumor of cecum in patient treated with imatinib mesylate for blastic phase of chronic myeloid leukemia Novaković Sabina, Kovač Peić Anamarija, Holik Hrvoje, Coha Božena. Acta Clinica Belgica.2017;72(6). CrossRef
- Case report and literature review: a rare patient with chronic myeloid leukemia and chronic lymphocytic leukemia Bhagavathi S, Borromeo V, Desai H, Crisan D. Ann Clin Lab Sci.2008;38(4):405-409.
- Successful management of synchronous recurrent breast carcinoma with chronic myelogenous leukemia: a case report Elm’hadi Choukri, Khmamouche Mohamed Reda, Tanz Rachid, Toreis Mehdi, Mahtat ElMehdi, Allaoui Mohammed, Oukabli Mohammed, Messaoudi Nezha, Errihani Hassan, Ichou Mohammed. Journal of Medical Case Reports.2017;11(1). CrossRef
- Secondary breast carcinoma after completely remitted chronic myeloid leukemia following targeted tyrosine kinase inhibitor therapy Pan Linlin, Duan Junwu, Qiao Weiqiang, Bi Lirong, Wu Di, Fan Zhimin, Yang Ming. Breast Cancer.2017;24(6). CrossRef
- Kaposi's sarcoma in a patient treated with imatinib mesylate for chronic myeloid leukemia Campione Elena, Diluvio Laura, Paternò Evelin J., Di Marcantonio Dely, Francesconi Arianna, Terrinoni Alessandro, Orlandi Augusto, Chimenti Sergio. Clinical Therapeutics.2009;31(11). CrossRef
- Osteoid osteoma transformation into osteoblastoma: Fact or fiction? Chotel F., Franck F., Solla F., Dijoud F., Kohler R., Berard J., Abelin Genevois K.. Orthopaedics & Traumatology: Surgery & Research.2012;98(6). CrossRef
- Computed tomography of axial skeletal osteoid osteomas Gamba JL, Martinez S, Apple J, Harrelson JM, Nunley JA. American Journal of Roentgenology.1984;142(4). CrossRef
- [Osteolytic lesions in chronic myeloid leukemia. Report of three cases (author’s transl)] Juncá Piera J, Durán Suárez JR, Triginer Boixeda J. Med Clin (Barc).1981;76(6):259-261.
- Solitary Lytic Bone Lesion in an Adult with Chronic Myelogenous Leukemia Nesbitt James, Roth Robert E.. Radiology.1955;64(5). CrossRef
- Osteolytic lesions in chronic granulocytic leukemia: a report of four cases Rizzo SC, Fontana G, Ricevuti G, Balduini CL. Haematologica.1977;62(1):61-74.
- Chronic Myeloid Leukemia with Osteolytic Bone Involvement [Internet]. [cited 2021 May 26] Available from: https://www.japi.org/v2e4b464/chronic-myeloid-leukemia-with-osteolytic-bone-involvement..
- Intracortical Bone Metastasis Mimicking Intracortical Osteoid Osteoma: A Case Report. undefined [Internet] Shin YR, Kim J. 2007 [cited 2021 May 26]; Available from: /paper/Intracortical-Bone-Metastasis-Mimicking-Osteoid-A-Shin-Kim/f322e1ae0dcd531f2ef5327d9b5b8490857c413c..
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2021
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times