Experience with Neuroendocine Carcinoma of Esophagus – A Decade at a Tertiary Care Centre in South India
Download
Abstract
Background: Esophageal neuroendocrine carcinoma (NEC) is a rare and aggressive malignancy with limited data on clinicopathologic features, treatment outcomes, and prognostic factors. This study aims to evaluate the clinical and pathological characteristics, survival outcomes in patients with esophageal NEC.
Methods: A retrospective analysis was conducted from 2012 to 2024 at our institute. All patients who were diagnosed with esophageal NEC were identified through the electronic medical records. Data on demographics, tumor characteristics, treatment modalities, and outcomes were collected. Progression-free survival (PFS) and overall survival (OS) were analyzed using Kaplan-Meier methodology, and subgroup analyses were performed to assess the impact of histological subtypes and treatment approaches.
Results: The cohort included 12 males and 12 females, with a mean age of 56 years (SD: ±11 years). The most common tumor locations were the mid (38%) and lower thoracic esophagus (33%). Median PFS and OS were 5 months (SD: ±3.9 months) and 6.3 months (SD: ±5.5 months), respectively. Most common modality of treatment was palliative chemotherapy for metastatic patients and concurrent chemo radiotherapy for non-metastatic patients. At the last follow-up, 75% of patients had succumbed to the disease, highlighting its aggressive nature.
Conclusions: Esophageal NEC is characterized by poor survival outcomes despite multimodal therapy. The findings underscore the need for prospective studies and novel therapeutic approaches, including targeted therapies and immunotherapy, to improve outcomes for this rare malignancy.
Introduction
High-grade neuroendocrine carcinoma (NEC) of the esophagus is a rare but aggressive malignancy, characterized by a poor prognosis and limited treatment outcomes. Current knowledge about clinicopathological features and survival outcomes in esophageal NEC is largely based on limited case studies and retrospective analyses [1, 2]. Moreover, the prognostic implications of mixed histology, combining neuroendocrine (large cell and small cell) are not well established.
Esophageal NEC often presents with advanced locoregional or distant metastasis at diagnosis, highlighting its aggressive nature. The esophagus, being a frequent site for gastrointestinal neuroendocrine tumors, adds further complexity to the diagnostic and therapeutic landscape. Understanding the differences in survival outcomes for NEC and other histologies is critical to tailoring effective treatment strategies [3].
In this study, we retrospectively evaluated the clinicopathological features, patterns of care and their outcomes of esophageal NEC over a decade at our institute. Our findings aim to contribute to the growing body of evidence needed for improved management of this rare but formidable malignancy.
Materials and Methods
This retrospective study included patients diagnosed with neuroendocrine carcinoma (NEC) of the esophagus, treated at our institution between 2012 to 2024. Data were extracted from institutional digital and case records to analyze clinicopathological features, treatment modalities, and survival outcomes. Inclusion criteria required histological confirmation of NEC, detailed treatment records, and available follow-up data of minimum 6 months. Clinical and demographic data, including age, sex, performance status (PS), comorbidities, and habits (e.g., smoking, alcohol consumption, tobacco use), were collected (Table 1).
| Age | |
| <50 | 6 |
| 50-70 | 16 |
| >70 | 2 |
| Sex | |
| Male | 12 |
| Female | 12 |
| PS | |
| 0 | 0 |
| 1 | 20 |
| 2 | 3 |
| 3 | 0 |
| 4 | 1 |
| Habits | |
| Alcohol | 15 |
| Tobacco usage | 12 |
| Co Morbids | |
| Diabetes mellitus | 8 |
| Systemic hypertension | 15 |
| Others | 0 |
Presenting symptoms, tumor location, histological subtype, IHC markers used and staging details were documented. Further patients were classified based on Tumor locations and metastatic or non metastatic at presentation (Table 2, 3).
| Small Cell | 20 |
| Large Cell | 2 |
| Combined | 2 |
| Less Than 70% | 4 |
| More Than 70% | 20 |
Treatment modalities included chemoradiation or palliative systemic therapy (Table 4).
| Location | |
| Midthoracic Esophagus | 10 |
| Lower Thoracic Esophagus | 12 |
| OG Junction | 2 |
| Length of Tumor | |
| Less than 5CM | 7 |
| 5-10 CM | 11 |
| More than 10CM | 6 |
| Localised Disease | 10 |
| Metastatic Disease | 14 |
For patients undergoing chemoradiation, radiation doses ranged between 50 to 60Gy with or without etoposide and platinum-based chemotherapy (Table 5, 6).
| Etoposide, Cisplatin | 12 |
| Etoposide, Carboplatin | 6 |
| Others | 6 |
| RT Technique | N |
| 3D CRT | 8 |
| IMRT | 1 |
| VMAT | 1 |
| Median RT Dose (Gy) | 50 |
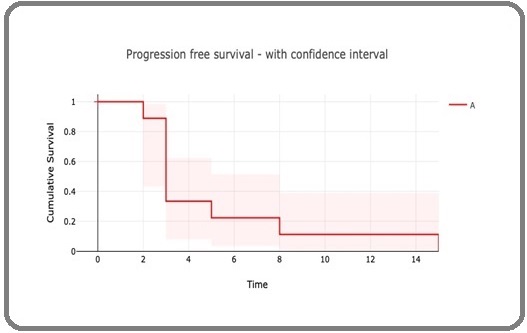
Progression-free survival (PFS) was calculated from the start of treatment to the first documented progression. Overall survival (OS) was measured from diagnosis to death due to any cause or last follow-up (Figure 1 and 2).
Figure 1. Overall Survival.
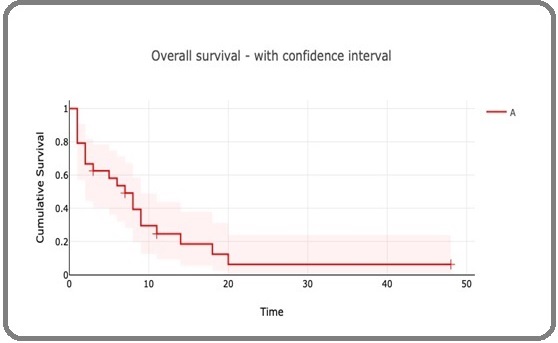
Figure 2. Progression Free Survival.
Statistical Analysis
Descriptive statistics summarized patient demographics, tumor characteristics, and treatment outcomes. Kaplan-Meier analysis was used to estimate survival curves, with differences assessed using the log-rank test. Statistical significance was defined as p<0.05 Analyses were performed using SPSS software.
Results
A total of 24 patients were included in the study, with an equal distribution of males and females (50% each). The mean age at diagnosis was 56 years (SD: ±11 years. The majority of patients had a performance status (PS) of 1 (83%), while a smaller subset had a PS of 2 (8%) or 4 (4%). The most common tumor location was the mid-thoracic esophagus (38%), followed by the lower thoracic esophagus (33%) and distal esophagus (17%). Tumors involving the gastroesophageal junction (OGJ) contributed for 8%. One case involved both the mid and lower thoracic esophagus. The median progression-free survival (PFS) was 5 months (SD: ±3.9 months), while the median overall survival (OS) was 6.3 months (SD:±5.5 months). Survival outcomes were generally poor, reflecting the aggressive nature of esophageal NEC. Recurrence was reported in five patients, with the most common sites being the locaoregional recurrence followed by brain. At the last follow-up, 18 patients (75%) were deceased, 2 patients (8%) were alive, 1 patient (4%) was lost to follow-up, and 1 patient (4%) was noted as living in clinical records.
Discussion
Esophageal neuroendocrine carcinoma (NEC) is a rare and aggressive malignancy with distinct clinical, histological, and prognostic features. The results of our study largely align with existing literature, while also highlighting some unique characteristics within our cohort.
The mean age of diagnosis in our cohort was 56 years, consistent with findings from global studies. Maru et al. and Ku et al. reported similar mean ages in their cohorts, typically ranging between 55 and 65 years [2, 3]. This age distribution underscores the tendency of NEC to present in older adults, which is likely associated with cumulative environmental exposures and comorbidities [2, 3]. However, cases have also been reported in younger individuals, emphasizing the variable age spectrum of this disease.
In contrast to the male predominance reported in most studies, such as those by Hudson et al. and Yun et al., where men accounted for 60–80% of cases, our cohort showed an equal gender distribution [4, 5]. This divergence may reflect regional differences in risk factors, such as smoking, alcohol use, and occupational exposures, which are traditionally higher in men. It also suggests the need for further studies to explore sex-based biological or environmental determinants in esophageal NEC.
Comorbid conditions were present in several patients in our cohort, including hypertension, diabetes, and obesity. While these are common in older populations, the impact of these conditions on the prognosis of esophageal NEC is less clear. Maru et al. did not identify specific comorbidities as prognostic factors, but their role in influencing treatment tolerance and outcomes warrants further investigation. Future studies could benefit from a detailed analysis of the interplay between comorbidities and disease progression.
The most common tumor sites in our cohort were the mid-thoracic (38%) and lower-thoracic esophagus (33%), consistent with global trends. Yun et al. and Maru et al. similarly reported that the mid and distal esophagus are the predominant sites for NEC. This distribution may reflect the proximity of these regions to the gastroesophageal junction, where the cellular environment may predispose to neuroendocrine differentiation [6-8].
The majority of our patients had a performance status (PS) of 1, indicating mild functional impairment. This aligns with observations in other studies, such as those by Ku et al., where most patients presented with manageable performance status at diagnosis. However, patients with a poorer PS, as seen in a small subset of our cohort, often had worse outcomes, emphasizing the importance of baseline functional status in guiding treatment decisions and predicting prognosis [9, 10].
Patients with mixed histology (NEC with adenocarcinoma or squamous carcinoma components)in our study had better outcomes compared to those with pure NEC, echoing findings by Maru et al.. The presence of mixed histology may indicate a less aggressive tumor biology, as the non-NEC component retains sensitivity to conventional treatments. Conversely, pure NEC was associated with more advanced disease at presentation and poorer outcomes, consistent with observations in the global literature.
Treatment outcomes in our cohort were modest, with median overall survival (OS) of 6.3 months and progression-free survival (PFS) of 5 months. These figures align with survival durations reported in studies by Hudson et al. and Casas et al., emphasizing the limited efficacy of current multimodal therapies. Chemoradiation, the mainstay treatment for most patients in our cohort, was associated with high rates of residual disease and recurrence. Surgical resection, performed in select cases with locoregional disease, showed limited survival benefit, as seen in other studies [11, 12].
Emerging therapies, including molecular-targeted agents and immunotherapy, have shown promise in other neuroendocrine tumors and may offer new avenues for treatment. While not yet widely adopted for esophageal NEC, preliminary evidence supports their potential efficacy, as highlighted in studies by La Rosa et al. [12]. Our study is limited by its retrospective design and small sample size. The lack of molecular data also restricts our understanding of disease biology and the potential for targeted therapies. Future prospective trials incorporating molecular profiling and novel treatment approaches are critical to improving outcomes for esophageal NEC.
In conclusion, Esophageal neuroendocrine carcinoma (NEC) is a rare and aggressive malignancy with poor prognosis, particularly in patients presenting with advanced disease. Our study underscores the challenges associated with managing this disease, with limited survival benefits despite multimodal therapy. Patients with mixed histology appear to have better outcomes, suggesting that the presence of a non-NEC component may influence prognosis favorably. However, the high recurrence rates and treatment resistance highlight the urgent need for novel therapeutic strategies, including molecular-targeted approaches and immunotherapy. Collaborative efforts and prospective studies are essential to enhance understanding and improve outcomes for patients with this challenging malignancy.
Acknowledgments
Statement of Transparency and Principals:
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Clinical Presentation and Diagnosis of Neuroendocrine Tumors Vinik AL , Chaya C. Hematology/Oncology Clinics of North America.2016;30(1). CrossRef
- Retrospective study of clinicopathologic features and prognosis of high-grade neuroendocrine carcinoma of the esophagus Maru DM , Khurana H, Rashid A, Correa AM , Anandasabapathy S, Krishnan S, Komaki R, Ajani JA , Swisher SG , Hofstetter WL . The American Journal of Surgical Pathology.2008;32(9). CrossRef
- Epidemiology of gastroenteropancreatic neuroendocrine tumours Fraenkel M., Kim M. K., Faggiano A., Valk G. D.. Best Practice & Research. Clinical Gastroenterology.2012;26(6). CrossRef
- Primary Small Cell Carcinoma of The Esophagus - An Eight Year Retrospective Study Nayal B, Vasudevan G, Rao ACK , Kudva R, Valliathan M, Mathew M, Rao L. Journal of clinical and diagnostic research: JCDR.2015;9(5). CrossRef
- The clinical features and treatment modality of esophageal neuroendocrine tumors: a multicenter study in Korea Lee CG , Lim YJ , Park SJ , Jang BI , Choi SR , Kim JK , Kim Y, et al . BMC cancer.2014;14. CrossRef
- Small-cell carcinoma of the gastrointestinal tract: a retrospective study of 64 cases Brenner B., Shah M. A., Gonen M., Klimstra D. S., Shia J., Kelsen D. P.. British Journal of Cancer.2004;90(9). CrossRef
- Clinicopathological Profile of Pure Neuroendocrine Neoplasms of the Esophagus: A South Indian Center Experience Babu Kanakasetty G, Dasappa L, Lakshmaiah KC , Kamath M, Jacob LA , Mallekavu SB , Rajeev LK , et al . Journal of Oncology.2016;2016. CrossRef
- A retrospective study of different treatments of limited-stage small-cell esophageal carcinoma and associated prognostic factor analysis Ding J., Ji J., Zhu W., Zhou K., Han J., Zhang Y., Yu C., et al . Diseases of the Esophagus: Official Journal of the International Society for Diseases of the Esophagus.2013;26(7). CrossRef
- Radiotherapy and chemotherapy are associated with improved outcomes over surgery and chemotherapy in the management of limited-stage small cell esophageal carcinoma Meng M, Zaorsky NG , Jiang C, Tian L, Wang H, Liu C, Wang J, et al . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2013;106(3). CrossRef
- Progress in the treatment of esophageal neuroendocrine carcinoma Ma Z, Cai H, Cui Y. Tumour Biology: The Journal of the International Society for Oncodevelopmental Biology and Medicine.2017;39(6). CrossRef
- Small cell carcinoma of the esophagus. Analysis of 14 cases and literature review Hosokawa A, Shimada Y, Matsumura Y, Yamada Y, Muro K, Hamaguchi T, Igaki H, et al . Hepato-Gastroenterology.2005;52(66).
- Neuroendocrine Carcinomas of the Gastroenteropancreatic System: A Comprehensive Review Ilett EE , Langer SW , Olsen IH , Federspiel B, Kjær A, Knigge U. Diagnostics (Basel, Switzerland).2015;5(2). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Environment and Cancer , 2026
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times