Analysis of Cone Beam CT based inter Fractional Set up Errors in Intensity Modulated Radiotherapy and Need for Safety Margins in Head and Neck Cancer Patients: An Institutional Experience
Download
Abstract
Background: The efficacy of IMRT depends on the patient’s set up during each fraction, ideal treatment set up results in better tumor volume coverage and minimal toxicities to surrounding normal structures. random set up errors are the prevalent ones. Cone beam CT is a method of developing a volumetric image guiding system allowing better assessment of treatment set up errors.
Purpose: The aim is to evaluate and quantify inter-fraction set up errors in the IMRT treatment and to decide adequate margins for the target volumes in head and neck cancer patients Method: A total of 300 CBCTs were performed and analysed in 50 patients of head and neck carcinoma. Set up verifications were done using KV-CBCT, taken on first 3 consecutive days of treatment; followed by weekly CBCTs for 3 weeks. Systemic corrections were done on day 3 after treatment initiation. The mean and range for random and systemic errors, as well as safety margins were calculated.
Results: The shifts were reduced after systemic correction to 1.46mm, 1.46mm and 1.70mm respectively. Transitional shifts more than 2.5 mm were seen in 46%, 42% and 34% of cases in ML, AP and SI directions, whereas it was seen in 12%, 14% and 8% of cases after systemic corrections. After systemic correction, the adequate PTV margin was found to be 3 mm, to compensate for set up errors.
Conclusion: This study suggested that CBCT for initial 3 consecutive days is sufficient to overcome set up errors, provided that systemic corrections are done if mean set up errors are >2.5 mm.
Introduction
Head and neck carcinoma are one of common causes of morbidity [1] and mortality. Squamous cell carcinoma being the most common histological variant, mostly arises from the mucosa of upper aero-digestive tract [2]. Radiation therapy plays a vital role in its management, not only in the terms of the dose delivery system with the particle therapy, but also in the patient immobilisation accuracy and precise tumour targeting. With the development and preference of IMRT [3, 4], SBRT, and RAPID Arc, the efficacy of dose delivery in terms of homogeneity, conformity and monitor units has improved over the years, but it also comes at the cost of increased chances of targets being missed [5, 6]. The tumour localisation at the time of simulation is the most basic and crucial step in the entire process of radiation therapy. The tumour target localisation is done prior to each fraction assuring the accurate dose delivery. It helps in deciding margins around target volumes and OARs, tells about efficacy of the immobilisation devices, probability and quantity of set up errors and assures targeted delivery of radiation. With increase in use of simultaneous integrated boost (SIB) and high-dose hypo-fractionation schedules, the cushion of set up error and margins around volumes have decreased and thus the need of guided delivery is much more needed. Addition of the imaging techniques along with the standard dose delivery system results in image guided radiation therapy [7] (IGRT).
With advent in technology, the demand of IGRT is escalating more than ever, as to overcome the errors occurring during radiation beam delivery or in between treatment fractions. The intra-fraction error are mostly because of physiological organ motions, breathing movements, and the inability to maintain treatment position everyday [8]. The inter-fraction errors are the set up errors or the issue in reproducing treatment position on couch by the patient. The set up errors, which include both systemic and random errors along with organ motion results into target miss, iso-centre miss or treatment related uncertainties. Organ motion have major role in thorax, abdominal and pelvic tumours and the set up errors are important in head and neck, cranium and limb situated tumours [9].
In order to reduce these errors, motion control and tracking devices, tumour location guiding devices are taken into use. Another method of reducing set up errors is by creating a margin around the target volume. Addition of margin to counteract set up errors and verifying it with the help of appropriate imaging system results in quantification and assessments of error margins.
Conventionally, this set up verification has been done with Kilo-voltage or megavoltage portal images. In recent times with the development of volumetric arc, it is done with cone beam computed tomography [10-12].
In most of the institutions, the protocol is localisation of the iso-centre on the thermoplastic mould and it causes a high probability of set up errors. The systemic errors can also be reduced by 3-5 [13-16] consecutive day verifications of matching the target volume with the help of portal images [17-19].The inter-fraction random errors are the ones that costs us the most and decides the margin. In our study, we analysed inter-fractional set-up verification for initial 3 consecutive days and then weekly for 3 weeks in the treatment of 50 head and neck cancer patients. The aim of this study was to quantify the set-up accuracy, assess the efficacy of the CBCT portal imaging and to confirm the sufficiency of standard 5 mm PTV margin to counteract the set up errors in head and neck cancer patients treated with IMRT.
Materials and Methods
A total of 50 histologically confirmed head and neck cancer patients were taken into the study and analysed (Table 1).
| Frequency | Percentage | |
| Age | 58 (35-73) | |
| Gender | ||
| Female | 21 | 42 |
| Male | 29 | 58 |
| Stage | ||
| II | 13 | 26 |
| III | 18 | 36 |
| IVA | 19 | 38 |
| Site | ||
| Oral cavity | 20 | 40 |
| Nasopharynx | 9 | 18 |
| Oropharynx | 6 | 12 |
| Hypo-pharynx | 7 | 14 |
| Parotid gland | 2 | 4 |
| Nasal cavity | 1 | 2 |
| Larynx | 5 | 10 |
| Histology (differentiation)- Squamous cell carcinoma | ||
| Well | 22 | 44 |
| Moderate | 13 | 26 |
| Poorly | 15 | 30 |
| Radiotherapy | ||
| Adjuvant RT | 38 | 76 |
| Definitive RT | 12 | 24 |
| Concurrent chemotherapy (Cisplatin) | ||
| Yes | 42 | 84 |
| No | 8 | 16 |
After complete work up of the patient, including, physical, pathological and radiological studies, patients were planned and taken up for radiotherapy. All the patients in the study received concurrent weekly cisplatin 40 mg/m2, along with ongoing radiotherapy as per NCCN guidelines.
Radiotherapy was delivered by intensity modulated radiation therapy technique. Patients were positioned in supine and immobilised with the help of head support pad using thermoplastic mask and shoulder retractors. They were scanned from mid chest to vertex in “G HIGH SPEED” CT simulator. Laser marks were marked on thermoplastic mould to define reference points according to the target volume to be treated. Contrast (IOHEXOL) was given intravenously to delineate cervical nodes. CT images were taken with slice thickness of 2.5 mm and were transferred to TPS “ECLIPSE”.
Contouring was done in accordance with ICRU 62 [20].
GTV: macroscopic disease including all positive lymph nodes.
CTV: subclinical disease present around gross tumour.
CTVgross: GTV +10 mm margin, removed from nearby critical structures.
PTV: 5mm expansion of CTV to account for potential setup error and motion [21].
Three PTVs were generated with different dose. PTV 70: High risk PTV
PTV 59.4: Intermediate risk PTV PTV 54: Low risk PTV
The prescribed doses were delivered in 33 fractions, five fractions per week from Monday to Friday, using IMRT-SIB technique [22].
IMRT treatment plans were created using 6 MV photons commissioned on a ‘True Beam’ with MLCs of 5 mm width, maximum speed of 2.5 cm/sec with variable dose rate of 600 MU/min and maximum field size of 40x40 cm2. Once the plan was prepared, the coordinates were sent to system software and the patient was shifted on the treatment couch. The final target coordinates were documented and confirmation of the target matching was done with KV CBCT. Isocentres were marked on thermoplastic mould after confirmation. The treatment fraction was delivered along with a check on systemic set up error by analysing KV CBCT. It was repeated in the similar manner for the next 3 consecutive days. The displacements were observed in all 3 axes; medio-lateral, antero-posterior and superior-inferior, which were recorded and corrected. If the average values of correction were more than 2.5 mm, systemic set up corrections were performed.
Subsequently, weekly KV CBCT were done to look for any random error during the treatment. The values were recorded, and if there were any discrepancies found in the alignment, they were corrected, and portal image matching were done on the subsequent days as well. Weekly quality assurance (QA) were performed regarding planning, immobilisation, and positioning and monthly quality assurance of mechanical system and image quality. Geometrical accuracy tests that verifies the CBCT reconstruction centres if they coincide with the isocentre of the linear accelerator, were performed on a weekly basis. The mean, range, and standard deviation were statistically assessed. Upon calculations of mean and standard deviation, systemic errors and random errors were calculated. The data were entered into an excel spreadsheet and were analysed using SPSS (version 25.0). Based on Van Herk formula, margins were added to CTVs to obtain PTVs and were calculated ensuring adequate CTV coverage (V95%>90%).
Van Herk formula (2.5∑ + 0.7r) where “∑” is systemic error and “r” is random error [23].
Results
A total of 300 CBCT scans were analysed from the first day of treatment to the completion of treatment. At the initiation of treatment, CBCTs were analysed for 3 consecutive days, after which weekly assessments were done. Further imaging were done, if required.
The mean set up error on Day 1 prior to treatment were 0.26 cm, 0.27 cm, 0.27 in mediolateral, antero-posterior and superior-inferior directions respectively. The range of errors were 0-7 mm in ML direction, 0-7 mm in AP and 0-8 mm in SI directions. A total of 11, 12 and 10 CBCTs out of 50 had translational shift of more than 2.5 mm in ML, AP and SI direction respectively, whereas amongst them 3, 4 and 4 had shift of more than 5mm. The translational shifts were corrected whenever they were greater than 2.5 mm (Table 2) (Figure 1).
| Day 1 | Day 2 | Day 3 | |||||||
| Medio- lateral | Antero- posterior | Super- inferior | Medio- lateral | Antero- posterior | Super- inferior | Medio- lateral | Antero- posterior | Super- inferior | |
| Mean (cm) | 0.26 | 0.27 | 0.27 | 0.21 | 0.19 | 0.19 | 0.17 | 0.12 | 0.13 |
| Range (mm) | 0-7 | 0-7 | 0-8 | 0-5 | 0-4 | 0-6 | 0-4 | 0-4 | 0-3 |
| Translational shift >2.5 mm | 11 | 12 | 10 | 8 | 7 | 5 | 4 | 2 | 2 |
| Translational shift >5mm | 3 | 4 | 4 | 1 | 0 | 1 | 0 | 0 | 0 |
Figure 1. Comparison of Translational Shifts in Medio-lateral (ML), Antero-posterior (AP), Superior-inferior (SI) directions on initial three consecutive days CBCTs.
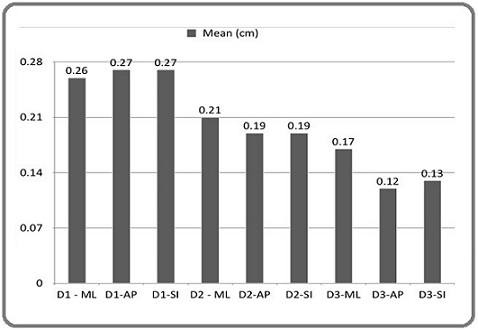
On 2nd day, mean translational shifts were 0.21cm, 0.19 cm and 0.19 cm, ranges were 0-5 mm, 0-4 mm and 0-6 mm respectively. Out of 50 CBCTs taken on that day, 8, 7 and 5 had translational shifts of more than 2.5mm and 1, 0 and 1 had shifts of more than 5mm in ML, AP and SI direction respectively. Similarly, as the previous day, shifts of more than 2.5 mm were corrected.
On 3rd day, mean translational shifts were 0.17 cm, 0.12 cm and 0.13 cm respectively in ML, AP and SI direction. The translational shifts ranged from 0-4 mm, 0-4 mm and 0-3 mm. 4, 2 and 3 patients had translational shift of more than 2.5 mm while none of them were greater than 5 mm in ML, AP, and SI direction.
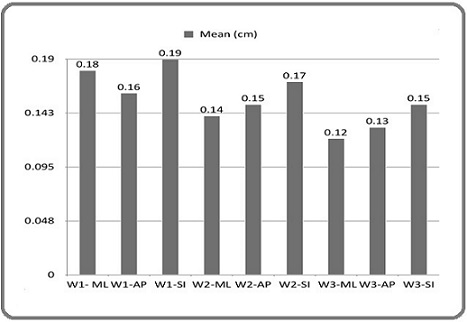
On third day as well, corrections were done only when translational shifts were more than 2.5 mm. If mean errors of the three days combined together had value more than 2.5mm, systemic set up error corrections were performed. On completion on 1st week, mean translational shifts were 1.8 mm, 1.6 mm, and 1.9 mm with shifts ranging from 0-5, 0-5, and 0-3 in ML, AP and SI directions. There was a significant decrease in translational shifts as compared to CBCTs done prior to systemic correction. It was evident in the form of frequency of shifts which were reduced to 3, 4 and 2 (shifts >2.5 mm) and 1, 1, 0 (shifts >5 mm). Translational shifts on week 2 and 3 are given in Table 3. (Figure 2).
| Week 1 | Week 2 | Week 3 | |||||||
| Medio- lateral | Antero- posterior | Super- inferior | Medio- lateral | Antero- posterior | Super- inferior | Medio- latera | Antero- posterior | Super- inferior | |
| Mean (cm) | 0.18 | 0.16 | 0.19 | 0.14 | 0.15 | 17 | 0.12 | 0.13 | 0.15 |
| Range (mm) | 0-5 | 0-5 | 0-3 | 0-3 | 0-3 | 0-4 | 0-3 | 0-3 | 0-3 |
| Translational shift > 2.5 mm | 3 | 4 | 2 | 2 | 1 | 1 | 1 | 1 | 1 |
| Translational shift >5 mm | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Figure 2. Comparison of Translational Shifts in Medio-lateral (ML), Antero-posterior (AP), Superior-inferior (SI) directions on weekly CBCTs.
A total of 150 CBCTs were acquired prior and after systemic corrections. The mean translational shifts prior to systemic correction were 2.13, 1.93 and 1.96 in medio- lateral, antero-posterior and superior-inferior directions. These shifts were reduced after systemic correction to 1.46, 1.46 and 1.70 respectively. The frequency of shifts of >2.5 mm were also reduced after systemic correction which were a total of 61 out of 150 CBCTs (40.6%) prior to systemic correction and 17 out of 150 (11.3%) after corrections. Similarly, the shifts of >5 mm were 14/150 (9.33%) prior and 2/150 (1.33%) after systemic corrections (Table 4) (Figure 3).
| Prior systemic correction | After systemic correction | |||||
| Medio-lateral | Antero-posterior | Super-inferior | Medio-lateral | Antero-posterior | Super-inferior | |
| Total CBCTs | 150 | 150 | 150 | 150 | 150 | 150 |
| Mean (cm) | 2.13 | 1.93 | 1.96 | 1.46 | 1.46 | 1.7 |
| Range (mm) | 0-7 | 0-7 | 0-8 | 0-5 | 0-5 | 0-3 |
| Translational shift > 2.5 mm | 23 | 21 | 17 | 6 | 7 | 4 |
| Translational shift >5mm | 5 | 4 | 5 | 1 | 1 | 0 |
| Systemic error | 1.4 | 1.2 | 1.2 | 0.8 | 0.7 | 0.8 |
| Random error | 1.2 | 1.6 | 1.8 | 1.1 | 1.3 | 1.3 |
| PTV margin (mm) | 4.41 | 4.12 | 4.26 | 2.77 | 2.66 | 2.91 |
Figure 3. Comparison of Translational Shifts in Mediolateral ( ML), Antero-posterior (AP), Supero-inferior (SI) directions prior to after systemic corrections.
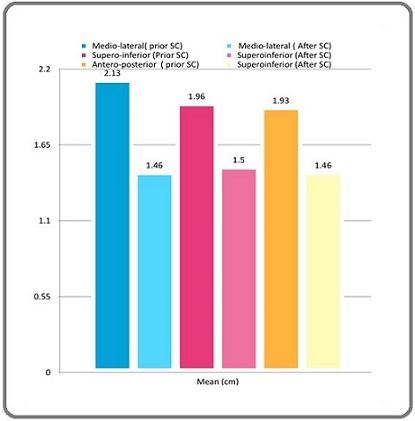
As shown in table 4, according to Van Herk formula, a margin of 5 mm is essential to be added to the CTVs in order to obtain PTV for compensating the set up errors. However, if systemic corrections are applied, the margins can be reduced to 3 mm.
Discussion
Various studies were performed in different tumour locations and they all suggested that CBCT is an effective application in evaluating set-up accuracy [24-28].
Dzierma et. al [24] concluded that set up corrections done in both Head and Neck and Prostate cancers were similar in planar and CBCT techniques. The set up margins calculated were 4.0 mm (AP), 3.8 mm (ML, SI) for head and neck cancer patients and 6.6 mm, 6.7 mm, 7.9 mm in SI, AP and ML directions respectively for Prostate cancer patients. This study suggested that set up margins added to CTV in the order to obtain 4 mm margin for HNCC and 6-8 mm for Prostate cancer.
Dionisi et al [25] analysed set up errors in 44 patients of HNCC with CBCT and they found that PTV margins were 3.48 mm, 4.33 mm and 4.08 mm in ML, AP and SI directions respectively before correction. However after correction, PTV margins were <2.5 m in all directions. They concluded that a margin of 5 mm to CTV to obtain PTV was safe in their treatment centre.
Wang et al [26] assessed set up errors in 22 patients of Nasopharyngeal carcinoma undergoing IMRT by using CBCT and found that pre-correction systemic errors ranged from 1.1-1.3 mm, and the random errors were also ranged from 1.1-1.3 mm. After online correction systemic errors reduced to 0.4-0.5 mm and random errors reduced to 0.7-0.8 mm in the three direction. The PTV margins were 3.5-4.2 mm in pre-correction position, 1.06-1.8 mm in pre-treatment position and 2.5-3.2 mm in post treatment position. They concluded that CBCT based online correction increased the accuracy of IMRT. Vidhi Jain et al [27] concluded in their prospective study of 100 patients (630 CBCTs) that set up errors >3mm and >5 mm were seen in 11.4% and 0.31%. The systemic errors and random errors prior to systemic correction were 1.0 mm, 1.1 mm, 1.2 mm and 2.4 mm, 2.0 mm and 2.1 mm in ML, SI and AP directions respectively. Systemic and random errors after correction were 0.6 mm, 0.7 mm, 0.7 mm and 1.3 mm, 1.0 mm, 1.2 mm in ML, SI and AP directions respectively. Study also concluded that CBCT at the first 3 fractions followed by weekly CBCT is an effective way to detect set up errors and a margin of 5 mm over CTV is safe to account for set up errors, however in special circumstances like close OAR, or with IGRT treatment modality, a PTV margin of 3 mm can be considered.
Similar to these studies, in our study of 50 patients with 300 CBCT acquired on first 3 treatment fractions followed by weekly CBCT for 3 weeks resulted that mean translational shifts prior to systemic correction were 2.13, 1.93 and 1.96 in mediolateral, anteroposterior and superior-inferior directions. These shifts were reduced after systemic correction to 1.46, 1.46 and 1.70 respectively. Systemic errors and random errors pre-correction were 1.4 mm, 1.2 mm, 1.2 mm and 1.2 mm, 1.6 mm, 1.8mm in ML, AP and SI directions respectively. These errors were 0.8mm, 0.7 mm, 0.8 mm and 1.1mm, 1.3 mm, 1.3 mm in ML, AP and SI directions respectively after systemic correction. The result of our study concluded that a margin of 5 mm over CTV can be given to account for set up errors and to obtain a safe PTV. In special circumstances, margins can be reduced to 3 mm, provided proper systemic corrections are applied after 3 initial consecutive CBCTs and if translational shifts are more than 2.5 mm.
The limitation of this study is that it does not account for different regions of interest and the number of patients were limited as this was an institutional study. Another fall out being that the CBCT verifications were acquired after systemic correction and not after every positioning. In conclusion, as we conclude from the study that
CBCTs are an efficient technique for quantification of systemic and random set up errors. It accounts for the efficiency of immobilisation devices and allows calculations of set up error margins from CTVs to PTVs. The margins added to CTVs to obtain PTVs were 5 mm in our treatment centre and research institute, which is safe for beam delivery for tumor treatment. Though it can be reduced in special circumstances, as in close proximity of OAR and systemic corrections, as and when needed. It was also summarized that acquiring CBCTs in the initial three consecutive days are sufficient to consider the interaction variability over the course of treatment.
Acknowledgments
Statement of Transparency and Principals
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research
References
- GLOBOCON 2020 worldwide .
- Oral cavity and oropharynx tumors Stambuk HE , Karimi S, Lee N, Patel SG . Radiologic Clinics of North America.2007;45(1). CrossRef
- Xerostomia and its predictors following parotid-sparing irradiation of head-and-neck cancer Eisbruch A., Kim H. M., Terrell J. E., Marsh L. H., Dawson L. A., Ship J. A.. International Journal of Radiation Oncology, Biology, Physics.2001;50(3). CrossRef
- EP-2092: Impact of treatment volumes in loco-regional failure of oral cancer in patients treated with IMRT Delishaj D , Ursino S , Lombardo E , Fatigante LR , Cantarella M, Coraggio G, Matteucci F, et al . Radiother Oncol.2016. CrossRef
- Inadequate target volume delineation and local-regional recurrence after intensity-modulated radiotherapy for human papillomavirus-positive oropharynx cancer Chen AM , Chin R, Beron P, Yoshizaki T, Mikaeilian AG , Cao M. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2017;123(3). CrossRef
- Dose variations in tumor volumes and organs at risk during IMRT for head-and-neck cancer Beltran M, Ramos M, Rovira JJ , Perez-Hoyos S, Sancho M, Puertas E, Benavente S, Ginjaume M, Giralt J. Journal of Applied Clinical Medical Physics.2012;13(6). CrossRef
- Intensity-modulated and image-guided radiation therapy for head and neck cancers Chu KP , Le Q. Frontiers of Radiation Therapy and Oncology.2011;43. CrossRef
- Quantifying the impact of respiratory-gated 4D CT acquisition on thoracic image quality: a digital phantom study Bernatowicz K., Keall P., Mishra P., Knopf A., Lomax A., Kipritidis J.. Medical Physics.2015;42(1). CrossRef
- Assessment of three-dimensional set-up errors in head and neck cancer patients treated by intensity modulated radiotherapy using electronic portal imaging device Bayoumi Y., Al-Amro A., Moniem R. A., Sohaibani I., Al-Hanafy O., Alawadi A. S., Asiri M.. The Gulf Journal of Oncology.2009;(6).
- Low-dose megavoltage cone-beam CT for radiation therapy Pouliot J, Bani-Hashemi A, Chen J, Svatos M, Ghelmansarai F, Mitschke M, Aubin M, et al . International Journal of Radiation Oncology, Biology, Physics.2005;61(2). CrossRef
- Megavoltage imaging, megavoltage cone beam CT and dose-guided radiation therapy Pouliot J. Frontiers of Radiation Therapy and Oncology.2007;40. CrossRef
- Different setup errors assessed by weekly cone-beam computed tomography on different registration in nasopharyngeal carcinoma treated with intensity-modulated radiation therapy Su J, Chen W, Yang H, Hong J, Zhang Z, Yang G, Li L, Wei R. OncoTargets and Therapy.2015;8. CrossRef
- Analysis of interfractional set-up errors and intrafractional organ motions during IMRT for head and neck tumors to define an appropriate planning target volume (PTV)- and planning organs at risk volume (PRV)-margins Suzuki M, Nishimura Y, Nakamatsu K, Okumura M, Hashiba H, Koike R, Kanamori S, Shibata T. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2006;78(3). CrossRef
- Evaluation of image-guidance protocols in the treatment of head and neck cancers Zeidan OA , Langen KM , Meeks SL , Manon RR , Wagner TH , Willoughby TR , Jenkins DW , Kupelian PA . International Journal of Radiation Oncology, Biology, Physics.2007;67(3). CrossRef
- Setup uncertainties of anatomical sub-regions in head-and-neck cancer patients after offline CBCT guidance Kranen S, Beek S, Rasch C, Herk M, Sonke J. International Journal of Radiation Oncology, Biology, Physics.2009;73(5). CrossRef
- Cone beam CT evaluation of patient set-up accuracy as a QA tool Nielsen M, Bertelsen A, Westberg J, Jensen HR , Brink C. Acta Oncologica (Stockholm, Sweden).2009;48(2). CrossRef
- Electronic portal image assisted reduction of systematic set-up errors in head and neck irradiation Boer H. C., Sörnsen de Koste J. R., Creutzberg C. L., Visser A. G., Levendag P. C., Heijmen B. J.. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2001;61(3). CrossRef
- Assessment of a customised immobilisation system for head and neck IMRT using electronic portal imaging Humphreys M, Guerrero Urbano MT , Mubata C, Miles E, Harrington KJ , Bidmead M, Nutting CM . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2005;77(1). CrossRef
- Multiple regions-of-interest analysis of setup uncertainties for head-and-neck cancer radiotherapy Zhang L, Garden AS , Lo J, Ang KK , Ahamad A, Morrison WH , Rosenthal DI , et al . International Journal of Radiation Oncology, Biology, Physics.2006;64(5). CrossRef
- Current ICRU definitions of volumes: limitations and future directions Purdy JA . Seminars in Radiation Oncology.2004;14(1). CrossRef
- Geometrical uncertainties, radiotherapy planning margins, and the ICRU-62 report Stroom JC , Heijmen BJM . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2002;64(1). CrossRef
- IMRT using simultaneously integrated boost (SIB) in head and neck cancer patients Studer G., Huguenin P. U., Davis J. B., Kunz G., Lütolf U. M., Glanzmann C.. Radiation Oncology (London, England).2006;1. CrossRef
- Errors and margins in radiotherapy Herk M. Seminars in Radiation Oncology.2004;14(1). CrossRef
- Set-up errors and planning margins in planar and CBCT image-guided radiotherapy using three different imaging systems: A clinical study for prostate and head-and-neck cancer Dzierma Y, Beyhs M, Palm J, Niewald M, Bell K, Nuesken F, Licht N, Rübe C. Physica medica: PM: an international journal devoted to the applications of physics to medicine and biology: official journal of the Italian Association of Biomedical Physics (AIFB).2015;31(8). CrossRef
- Set-up errors and planning target volume margins in head and neck cancer radiotherapy: a clinical study of image guidance with on-line cone-beam computed tomography Dionisi F, Palazzi MF , Bracco F, Brambilla MG , Carbonini C, Asnaghi DD , Monti AF , Torresin A. International Journal of Clinical Oncology.2013;18(3). CrossRef
- The clinical feasibility and effect of online cone beam computer tomography-guided intensity-modulated radiotherapy for nasopharyngeal cancer Wang J, Bai S, Chen N, Xu F, Jiang X, Li Y, Xu Q, et al . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2009;90(2). CrossRef
- A prospective study to assess and quantify the setup errors with cone-beam computed tomography in head-and-neck cancer image-guided radiotherapy treatment Jain V, Soni TP , Singh DK , Patni N, Jakhotia N, Gupta AK , Gupta TC , Singhal H. Journal of Cancer Research and Therapeutics.2023;19(3). CrossRef
- Quantification and Assessment of Interfraction Setup Errors Based on Cone Beam CT and Determination of Safety Margins for Radiotherapy Cubillos Mesías M, Boda-Heggemann J, Thoelking J, Lohr F, Wenz F, Wertz H. PloS One.2016;11(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Environment and Cancer , 2026
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times